Disc Replacement Surgery
Disc replacement surgery is an alternative treatment to spinal fusion surgery for a variety of spinal problems. It has been available for conditions of the cervical and lumbar spine since the 1960s in the form of crude, surgical steel ball-bearings. But over the last several decades, there has been renewed interest and rapid advancement in the technology and surgical techniques.
- What is disc replacement surgery?
- Who is a good candidate?
- What conditions does it treat?
- Which discs are commonly replaced?
- How is it performed?
- How long does the surgery take?
- What is the recovery time?
- What risks or complications can occur?
- How successful is this surgery?
- What are the alternatives?
What is disc replacement surgery?
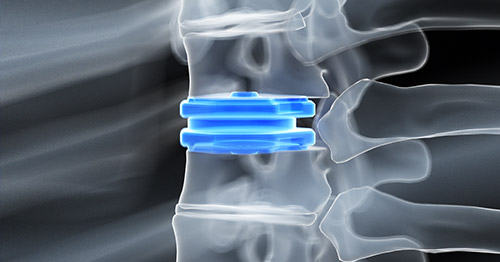
Disc replacement surgery involves removal of the diseased disc tissue and implantation of an artificial disc implant. There are cervical and lumbar disc replacement devices. The artificial disc is designed to preserve the natural motion of the spine while remaining securely fixed to the surrounding vertebral bones.
Total disc replacement is newer and performed less often than traditional spinal decompression and fusion surgeries. However, it is gaining favor for its ability to preserve motion while also treating neck or back pain as more long-term outcomes studies demonstrating its effectiveness become available.
Who is a good candidate for spinal disc replacement surgery?
One of the primary goals of disc replacement surgery is to preserve spinal motion. Patients with diseased discs in the cervical or lumbar spine who have good spinal motion and little or no arthritis are excellent candidates for disc replacement surgery. HSS research suggests that patients with greater height in their spinal discs may be better candidates than those with less disc height.
What conditions does disc replacement surgery treat?
Disc replacement therapy can be used to treat similar conditions to traditional spinal decompression and fusion surgeries, including pinched nerves associated with lumbar or cervical radiculopathy and myelopathy, and degenerative disc disease in both the cervical and lumbar spine.
Which spinal discs are most commonly replaced?
Cervical disc replacement is currently more popular than lumbar disc replacement surgery. The number of cervical disc replacement surgeries performed across the United States has increased nearly twofold as compared to the number performed around the year 2000, especially since around 2012. However, compared with traditional fusion procedures, it is still much less popular. Cervical and lumbar disc replacement is currently FDA approved for one and two-level surgeries.
How is a disc replacement performed?
Disc replacement surgery is performed differently depending on the region of the spine involved.
Cervical disc replacement
For cervical disc replacement, a small incision is made over the front of the neck. The soft tissues of the neck including the esophagus, trachea, and blood vessels are carefully protected and moved away from the spine. Once the appropriate spinal level is identified, the diseased disc is removed. The remaining bone above and below is prepared to receive the implant. The artificial disc is then implanted and secured to the bone. Placement is confirmed using X-ray.
Lumbar disc replacement
For lumbar disc replacement, surgeries may be performed with the assistance of a vascular or abdominal surgeon. An incision is made low over the front of the abdomen. The vital organs, blood vessels, and nerves are carefully protected and moved away from the front of the spine. Once the appropriate level is confirmed, the diseased disc is removed. The remaining bone above and below is prepared to receive the implant. The artificial disc is then implanted and secured to the bone. Placement is confirmed using X-ray.
Video: Animation of a lumbar disc replacement
Is disc replacement surgery painful?
Surgery for disc replacement surgery can be performed in a minimally invasive fashion, requiring little soft-tissue dissection in order to achieve an excellent result. Most patients are able to walk the same day as their surgery, both for cervical and lumbar procedures.
In select cases, patients can have this procedure as an outpatient, meaning you can recover at home the same day as your surgery. Your surgeon will work with our multidisciplinary services to ensure that you are comfortable after surgery.
What are artificial spinal discs made of?
There are several artificial disc devices available to surgeons at HSS. They will select the device that is most appropriate for your case. In general, devices are composed of surgical metals (such as surgical stainless steel or titanium) and specialized plastic bearings. The metal surfaces of the implants securely glide across the plastic bearings, replicating normal spinal motion.
How long does disc replacement surgery take?
Disc replacement surgery can be performed quickly compared to other spinal procedures because it does not involve preparing the bones for fusion. Surgical times can be roughly approximated to one to two hours per spinal level being addressed. Surgical duration can be variable, depending on the complexity of the individual case and should be discussed with your surgeon.
What is the recovery time for disc replacement surgery?
Patients can generally expect to spend at least one night in the hospital after disc replacement surgery. In select cases, these surgeries may be performed as an outpatient, allowing patients to recover at home the same day. There is typically no brace wear required, however this should be discussed with your surgeon. Normal activities of daily life such as sitting, standing, walking, bathing, etc. can be done right away. Rigorous or high impact activity is restricted until the surgical site is well healed, usually just a few weeks. Some patients may benefit from a short course of physical therapy afterwards. In general, patients can expect to return to normal activities three months after surgery.
What risks or complications can occur with disc replacement?
All surgeries carry some amount of risk, including infection, bleeding, and damage to important, nearby structures. These risks are very low and can be mitigated with excellent surgical technique. Compared with traditional fusion procedures there are unique risks to disc replacement due to the nature of the implants themselves. Because there are a variety of implants available, you should discuss these with your surgeon.
How successful is disc replacement surgery?
Disc replacement surgery can be performed in the cervical and lumbar spine and for a variety of conditions in each level. Success of the surgery depends on the condition being treated and numerous individual patient factors. Disc replacement surgery is generally successful in treating symptoms of radiculopathy, nerve pain that travels down the arms or legs. Disc replacement can be effective for neck and back pain, but this result is less reliable. You should discuss your treatment plan with your surgeon for a more detailed explanation of expected results.
What are the alternatives to artificial disc replacement surgery?
Alternatives to disc replacement surgery depend on the symptoms that you are experiencing. Pinched nerves or spinal stenosis can be treated with spinal decompression surgery. For patients with advanced degenerative disc disease and/or spinal arthrosis, a spinal fusion procedure may be more appropriate.
For example, anterior cervical discectomy and fusion (ACDF surgery) may be an alternative for cervical conditions causing neck or arm pain, while a transforaminal lumbar interbody fusion (TLIF surgery) may be an option for symptoms associated with lower back problems. Your surgeon will discuss which options may be appropriate for your condition.
The choice between these or any surgeries should be made based on the individual patient's needs and preferences. For some patients with neck problems, for example, either a disc replacement or an ACDF may be equally effective treatment options but with some possible trade-offs such as length of hospital stay.
Disc Replacement Surgery Success Stories
References
- Frelinghuysen P, Huang RC, Girardi FP, Cammisa FP Jr. Lumbar total disc replacement part I: rationale, biomechanics, and implant types. Orthop Clin North Am. 2005 Jul;36(3):293-9. doi: 10.1016/j.ocl.2005.02.014. PMID: 15950689.
- McCarthy MH, Louie PK, York PJ, Othman YA, Vaishnav AS, Sato K, Lee R, Huang RC, Albert TJ, Qureshi SA. Radiographic Evaluation of Cervical Disk Replacement: The Impact of Preoperative Arthrosis and Implant Positioning on Patient-report Outcomes. Clin Spine Surg. 2020 Nov;33(9):370-377. doi: 10.1097/BSD.0000000000001091. PMID: 33027091.
- Mok JK, Sheha ED, Samuel AM, McAnany SJ, Vaishnav AS, Albert TJ, Gang CH, Qureshi S. Evaluation of Current Trends in Treatment of Single-level Cervical Radiculopathy. Clin Spine Surg. 2019 Jun;32(5):E241-E245. doi: 10.1097/BSD.0000000000000796. PMID: 30762836.
- Othman YA, Verma R, Qureshi SA. Artificial disc replacement in spine surgery. Ann Transl Med. 2019 Sep;7(Suppl 5):S170. doi: 10.21037/atm.2019.08.26. PMID: 31624736; PMCID: PMC6778281.
- Paek S, Zelenty WD, Dodo Y, Sarin M, Shue J, Soffin EM, Cammisa FP, Girardi FP, Sama AA, Lyman S, Hughes AP. Up to 10-year surveillance comparison of survivability in single-level cervical disc replacement versus anterior cervical discectomy and fusion in New York. J Neurosurg Spine. 2023 Apr 21:1-10. doi: 10.3171/2023.3.SPINE221377. Epub ahead of print. PMID: 37086159.
- Phillips FM, Coric D, Sasso R, Lanman T, Lavelle W, Blumenthal S, Lauryssen C, Guyer R, Albert T, Zigler J, Cammisa F, Milam RA. Prospective, multicenter clinical trial comparing M6-C compressible six degrees of freedom cervical disc with anterior cervical discectomy and fusion for the treatment of single-level degenerative cervical radiculopathy: 2-year results of an FDA investigational device exemption study. Spine J. 2021 Feb;21(2):239-252. doi: 10.1016/j.spinee.2020.10.014. Epub 2020 Oct 21. PMID: 33096243.
- Shahi P, Vaishnav AS, Lee R, Mai E, Steinhaus ME, Huang R, Albert T, Iyer S, Sheha ED, Dowdell JE, Qureshi SA. Outcomes of cervical disc replacement in patients with neck pain greater than arm pain. Spine J. 2022 Sep;22(9):1481-1489. doi: 10.1016/j.spinee.2022.04.001. Epub 2022 Apr 8. PMID: 35405338.
- Shein D, Shue J, Girardi F. Evaluation of Aesculap Implant Systems activl Artificial Disc for the treatment of degenerative disc disease. Expert Rev Med Devices. 2016 Dec;13(12):1069-1072. doi: 10.1080/17434440.2016.1256771. Epub 2016 Nov 22. PMID: 27807981.
- Steinberger J, Qureshi S. Cervical Disc Replacement. Neurosurg Clin N Am. 2020 Jan;31(1):73-79. doi: 10.1016/j.nec.2019.08.009. Epub 2019 Oct 24. PMID: 31739932.
- Vaishnav AS, Gang CH, Iyer S, McAnany S, Albert T, Qureshi SA. Correlation between NDI, PROMIS and SF-12 in cervical spine surgery. Spine J. 2020 Mar;20(3):409-416. doi: 10.1016/j.spinee.2019.10.017. Epub 2019 Oct 31. PMID: 31678044.
Updated: 10/24/2023
Reviewed and updated by Frank P. Cammisa Jr., MD; and William D. Zelenty, MD