Osseointegration Limb Replacement
The HSS Osseointegration Limb Replacement Center at Hospital for Special Surgery provides a major advance in amputation reconstruction surgery for amputees who have not tolerated or do not want to use a traditional prosthetic socket. The interdisciplinary team of amputation reconstruction specialists, upper- and lower-extremity surgeons are devoted to helping amputees improve their mobility and daily lives. Hospital for Special Surgery is continually ranked #1 orthopedic hospital in the United States, and HSS surgeons were the first in the United States to perform osseointegration limb replacement for people with transtibial amputations.
What is osseointegration?
Osseointegration is the scientific term for bone ingrowth into a metal implant. An artificial implant is permanently, surgically anchored and integrated into bone, which then grows into the implant.
Osseointegration is most commonly used in dental implants and joint replacement surgery. It has been very successful in these uses for decades.
What is osseointegration limb replacement?
In this surgery, a limb prosthesis is connected directly to the skeleton. The prosthesis is a custom-made, porous, coated titanium implant that is aligned with the bone of the residual limb. (Find a doctor at HSS who performs osseointegration limb replacement.)
HSS was the first hospital in the United States to use osseointegration to treat people with transtibial amputations (below the knee).
Osseointegration limb replacement surgery can be done in the following bones:
- the femur (thighbone)
- tibia (leg bone)
- humerus (upper arm bone)
- radius and ulna (forearm bones)
What are the advantages of osseointegration over traditional prosthetic limbs?
In general, this procedure:
- improves mobility (control of the prosthetic leg)
- improves proprioception
- reduces nerve pain
- eliminates common problems associated with sockets
Patients with an osseointegrated limb have better physical control over – and a more intimate, emotional connection to – their prosthetic leg or arm, compared to those using a traditional socket prosthesis. The direct skeletal connection between the prosthesis and the patient’s own natural bone provides superior stability, strength and energy transfer (in which muscle strength from the residual limb is diminished where it connects with the prosthesis).
In particular, patients who have an osseointegrated prosthetic limb have dramatically improved proprioception, called osseoperception. Touch vibrations to the implant (such as during impact with the ground while walking) can be transferred through to the person’s natural bone. This helps patients walk more smoothly, feel more stable and effectively transfer all of the strength of their residual limb to the prosthesis.
Video: Wounded warrior stands tall after bilateral osseointegration limb replacement
Bone-anchored prostheses have been shown to lead to better patient outcomes than standard, socket-based prostheses. An osseointegrated prosthetic limb reduces or eliminates common problems associated with sockets, including:
- pinching
- sweating
- poor fit or need for frequent refitting
- poor ability to control the prosthesis
- lack of patient confidence due to mobility challenges
- nerve pain
- skin, irritation, sores and ulcers
In traditional prosthetic leg systems, there can be a poor fit between the residual limb and the socket. Many patients experience significant changes in the size and shape of their residual limb during the first 12 to 18 months after amputation surgery.
In addition, the angle at which the remaining leg bone rests inside the socket is frequently uneven with the prosthetic leg. This is called malalignment. Such awkward angles can cause balance problems and poor energy transfer. This can make it difficult for patients to move well and can even lead to falls and fractures.
Osseointegration procedural animations
Osseointegration limb replacement surgery for transfemoral amputation
Managing a tibia amputation with osseointegration reconstruction
Improved movement in the upper limbs
In patients with arm and hand prostheses, the large harness and socket that is often used in upper extremity prosthetics is eliminated. This enables the patient to actively use their body’s natural shoulder and elbow movement.
Osseointegrated arm implants are also compatible with myoelectric (bionic) prostheses. These allow muscle twitches in the residual arm to communicate with the arm prosthesis to allow patients to actively move their prosthetic elbow, wrist and hand. New technologies use pattern recognition algorithms to relay muscle movement signals in real time from the residual limb to the brain and then back to microcontrollers that control the movement of the bionic arm or hand. In some cases, targeted muscle reinnervation (TMR) is used to enhance the muscle signals.
Individual types of prosthetic limbs designed for different purposes, such as swimming or running, can be easily connected to and disconnected from the implant abutment using an Allen wrench (hex key) or quick-connect hardware.
Reduced nerve pain
Many amputees also experience nerve pain in the residual limb, which is caused by a neuroma. This is often described as “phantom” leg or arm pain. In most cases, wearing a socket prosthesis puts added pressure on the remaining limb, which worsens this nerve pain.
New surgical procedures to ease the pain associated with amputation neuromas can now also be performed together with osseointegration surgery. These include:
- targeted muscle reinnervation (TMR)
- regenerative peripheral nerve interface (RPNI) with free muscle graft
Who is a candidate for osseointegration limb replacement?
Osseintegration leg or arm replacment is especially helpful for amputees who are having a poor experience with their socket prosthesis.
The use of a socket is often especially difficult for patients whose residual limb is any of the following:
- short
- wide
- scarred
- painful
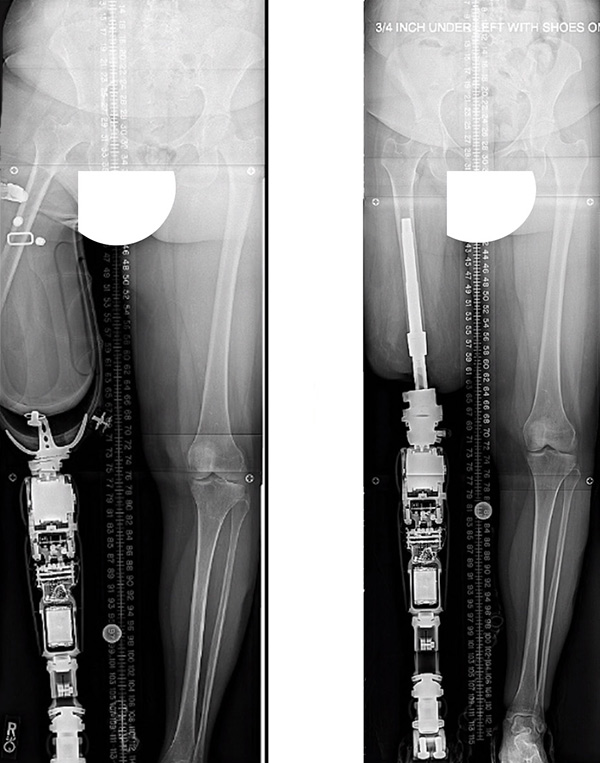
Before-and-after X-ray images showing malalignment between an above-the-knee amputation residual limb with a socket-based prosthesis (left); and an aligned, osseointegrated leg implant and connected prosthesis (right)
How is osseointegration limb replacement surgery done?
The process begins with front- and side-view X-rays and CT scans of the limb. These are taken to determine precise measurements for a custom-made implant built to fit inside the bone.
The implant is created and inserted into the residual limb bone and connected to a dual post, also known as a dual cone. The surgery to prepare and install the implant is done during a single hospital stay, rather than in separate surgeries. Surgeons also address any neuromas or problems with soft tissues and partner with plastic surgeons to perform soft-tissue contouring to enhance the benefits of limb replacement. This usually involves removing, lifting and tightening excess or loose soft tissue.
At HSS, we have assembled an interdisciplinary team of healthcare practitioners for osseointegration procedures. Each person plays an essential role in ensuring the best outcomes for the patient. The team includes:
- surgeons, anesthesiologists and nurses
- prosthetics professionals known as orthotists or prosthetists
- physical and occupational therapists

What is the recovery time for osseointegration surgery?
The average hospital stay is three to four days. The growth of the bone into the implant takes about three months. Most patients can walk without crutches within about three months after surgery.
Osseointegrated leg implant recovery: The first days and weeks
On the day after surgery, a rubber footie is applied to the end of the abutment, and patients can gradually put weight on the new implant. This “loading” process begins with 20 pounds of loading for 10 to 15 minutes, four to six times per day. Patients then use crutches and work with an outpatient physical therapist over several weeks to gradually increase weight loading until the prosthetic leg is attached.
After four days, patients can start a daily shower and clean the stoma with soap and water. For the first few weeks, the surgical area will be wrapped in gauze to prevent infection.
The prosthetic leg is attached to the implant between 3 to 10 weeks after surgery, depending on bone quality. After this, patients continue to use crutches for another six weeks.
Video: HSS patient Jesse Levine demonstrates connecting and disconnecting his osseointegrated leg prosthesis
What are the risks of osseointegration?
The odds of experiencing risks are low, but they can include:
- implant loosening
- fracture
- infection
Learn why HSS has exceptionally lower infection rates than many other hospitals.
To protect patients in case of a severe fall, the connection between the implant and the prosthesis has a fail-safe mechanism to protect the bone and implant. This is similar to ski bindings that automatically release during a fall.
How long does an osseointegrated prosthesis last?
The implant is expected to last for many years after successful osseointegration with the bone. Connection parts with the prosthetic may, over time, need to be changed by the prosthetist.
This procedure has been done in Sweden since 1990, but is relatively new, so there is not a lot of long-term results available. Implant designs have improved in recent years, and we expect these to function well over decades.
The need for revision surgery is possible in cases of fracture, loosening or deep infection.

Osseointegration Limb Replacement Success Stories
In the news
References
- Black, Grant G. BA; Wu, Xian MPH; Rozbruch, S. Robert MD; Otterburn, David M. MD: A Solution to Poorly Tolerated Lower Limb Amputations: Osseointegrated Prostheses Prove Cost-effective in the United States. Plastic and Reconstructive Surgery - Global Open: October 2021 - Volume 9 - Issue 10S - p 124, doi: 10.1097/01.GOX.0000799736.63628.5f.
- Hoellwarth JS, Al Muderis M, Rozbruch SR. Cementing Osseointegration Implants Results in Loosening: Case Report and Review of Literature. Cureus. 2020 Feb 21;12(2):e7066. doi: 10.7759/cureus.7066. PMID: 32226668; PMCID: PMC7089626.
- Hoellwarth Jason Shih, Geffner Adam Daniel, Reif Taylor J, Rozbruch SR. Transcutaneous osseointegration for amputees with short residual bone: Is there increased risk for complications? – A pilot study. Journal of Limb Lengthening & Reconstruction. Year : 2022 | Volume: 8 | Issue Number: 2 | Page: 115-120. DOI: 10.4103/jllr.jllr_22_22.
- Hoellwarth JS, Tetsworth K, Akhtar MA, Al Muderis M. The Clinical History and Basic Science Origins of Transcutaneous Osseointegration for Amputees. Adv Orthop. 2022 Mar 18;2022:7960559. doi: 10.1155/2022/7960559. PMID: 35340813; PMCID: PMC8956382.
- Hoellwarth JS, Tetsworth K, Rozbruch SR, Handal MB, Coughlan A, Al Muderis M. Osseointegration for Amputees: Current Implants, Techniques, and Future Directions. JBJS Rev. 2020 Mar;8(3):e0043. doi: 10.2106/JBJS.RVW.19.00043. PMID: 32224634; PMCID: PMC7161721.
- Jaime KM, Reif TJ, Kafedzic H, Garrison G, Dhawan J, Rozbruch SR. Attachment of a Myoelectric Prosthesis After Transulnar Osseointegration Implantation: A 2-Patient Case Study. JBJS Case Connect. 2021 Dec 15;11(4). doi: 10.2106/JBJS.CC.21.00381. PMID: 34910710.
- Marano AA, Modiri O, Rozbruch SR, Otterburn DM. Soft Tissue Contouring at the Time of Osseointegrated Implant Reconstruction for Lower Extremity Amputation. Ann Plast Surg. 2020 Jul;85(S1 Suppl 1):S33-S36. doi: 10.1097/SAP.0000000000002329. PMID: 32187066.
- Reif T.J., Fragomen A.T., Rozbruch S.R. (2022) Percutaneous Osseointegration Prosthesis. In: Özger H., Sim F.H., Puri A., Eralp L. (eds) Orthopedic Surgical Oncology For Bone Tumors. Springer, Cham. https://doi.org/10.1007/978-3-030-73327-8_26.
- Reif TJ, Khabyeh-Hasbani N, Jaime KM, Sheridan GA, Otterburn DM, Rozbruch SR. Early Experience with Femoral and Tibial Bone-Anchored Osseointegration Prostheses. JB JS Open Access. 2021 Sep 3;6(3):e21.00072. doi: 10.2106/JBJS.OA.21.00072. PMID: 34497971; PMCID: PMC8416017.
Updated: 1/10/2023
