Trigger Finger

Trigger finger (stenosing tenosynovitis) is one of the most common causes of hand disability, affecting between 1% and 2% of the population, and as high as 20% of people with high risk factors.
What is trigger finger?
Trigger finger is an irritation caused by thickening of a ligament at the base of the finger. The ligament forms a tunnel overlying the flexor tendon, which connects your forearm muscles to your finger bones and enables your fingers to flex (bend) and extend (straighten). A healthy flexor tendon glides smoothly through this tunnel called the flexor sheath. The tunnel is made of multiple ligaments called pulleys. Trigger finger specifically causes thickening at the first pulley (called A1), which is located where the finger meets the palm. When this becomes thickened, finger movements cause pain, and the flexor tendon can catch or even become locked in a bent position in severe cases.
What is trigger thumb?
Trigger finger can affect any of the five digits of the hand, but it most commonly occurs in the ring finger or the thumb. When the thumb the affected digit, it is simply sometimes referred to as “trigger thumb.”
What are the symptoms of trigger finger?
Signs and symptoms of trigger finger include pain or tenderness at the lowest joint on the palm side of the affected finger, a clicking, catching or snapping sensation while flexing or extending the finger. It may even become difficult to bending or, especially, straighten the finger. In some cases, the finger may become locked up in a bent position and must be gently opened using the other hand. People with trigger finger often report that their symptoms are worst when they first wake up in the morning.
(Find a doctor at HSS who diagnoses and treats trigger finger.)
What is the difference between trigger finger and Dupuytren’s contracture?
Like trigger finger, Dupuytren’s contracture can also cause an involuntary bent position of the fingers. But whereas trigger finger involves thickening of a ligament and, sometimes a tendon, in Dupuytren’s contracture, it is the fibrous tissue just under the skin called fascia that thickens and becomes tighter and shorter on the palm side of the fingers, causing inability to straighten fully. Dupuytren’s contracture is not as common as trigger finger and is associated with visible thickening of the tissue of the palm that cannot be seen in trigger fingers. Dupuytren’s contracture leads to inability to fully straighten the finger, but never causes a problem making a fist, whereas trigger finger may cause difficulty both straightening and bending the finger.
Can you get trigger finger in both hands at once?
Yes. Trigger finger can occur in one finger or multiple fingers, including on either hand at the same time.
What causes trigger finger?
The exact cause of trigger finger is unknown, however it is associated with repetitive gripping or squeezing hand motions as well as with certain medical conditions (comorbidities), including diabetes, rheumatoid arthritis, gout, pseudogout, sarcoidosis and hypothyroidism. Evidence suggests some people may also have a genetic predisposition for this condition.
Who is at risk for trigger finger?
Trigger finger most often appears in people between the ages of 40 and 60 and in women more so than men. It is more common among people who perform frequent or intense gripping in their work or leisure activities. At especially high risk are people with inflammatory disorders, including rheumatoid arthritis, gout and sarcoidosis, and in those who have an underactive thyroid or diabetes. Between 5% and 20% of diabetes patients will develop trigger finger.
Is there a trigger finger test? How is it diagnosed?
A physician usually diagnoses the condition without the need of imaging by taking a patient’s symptom history and doing a physical exam. Your doctor will touch your fingers as you open and close them, ask you about your pain during that motion, and check for signs of clicking or locking. If, while palpating the finger, your doctor detects nodules (swollen lumps) and thickening of the flexor tendon, this potentially indicates more advanced trigger finger.
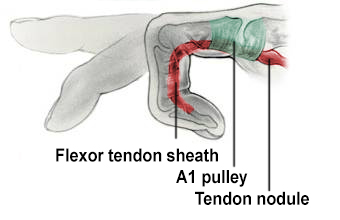
Illustration of trigger finger where the finger is locked in flexed position.
In some cases, ultrasound imaging may be warranted to understand all the physical dynamics associated with a person’s trigger finger and/or to determine whether other soft tissue conditions are also present.
What self-care or exercises can treat trigger finger?
You should consult a doctor if you suspect you have trigger finger, but self-care can begin at home. This may include identifying what recent activities involving making a fist may have brought it on and decreasing that activity for one to two weeks. For people who have worst symptoms in the morning, keeping the hand out of a fist overnight with a finger splint to hold the affected digit straight while sleeping may help. If a diagnosis of trigger finger is confirmed and surgery is not needed, a certified hand therapist can also teach you appropriate exercises for trigger finger, such as wrist stretches and fingertip bends. They may also advise you on using assistive devices to perform daily activities without stressing your flexor tendon
What is the treatment for trigger finger?
Most cases of trigger finger can be effectively managed without surgery with conservative measures. These may include modifying activity to rest the tendon, using a trigger finger splint that immobilizes the finger in a straightened position and/or, a corticosteroid injection. Corticosteroid injections are very safe and effective at curing trigger fingers in many patients, however repeated injections (more than two or three) should be avoided in the same finger to avoid potential complications.
Treatment may also include rehabilitation by a certified hand therapist (CHT). A hand therapist may employ physiotherapy techniques that include heat, massage, finger stretches and manual of the finger joints. They will also instruct you on trigger finger exercises to do at home.
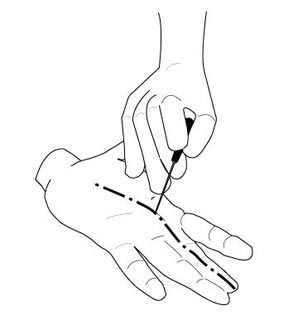
Illustration of percutaneous trigger finger release.
What is the surgery for trigger finger?
Conservative methods are attempted before offering surgery, but when nonoperative measures fail, surgical intervention should be performed swiftly to prevent the finger or thumb from becoming permanently flexed (bent). The quick procedure is called trigger finger release (or A1 pulley release) and may be with the use of numbing medicine with the patient awake or sedated.
Can trigger finger heal on its own?
Mild cases of trigger finger can resolve on their own. Trigger finger involving recurring or continuous pain, restricted mobility or a chronically bent figure will need treatment.
(Find a doctor at HSS who diagnoses and treats trigger finger.)
Articles related to trigger finger
Learn about associated and related conditions, and get a deeper dive on hand surgery treatments.
Trigger Finger Success Stories
References
- Kang L, Save AV. Hand Problems: Common Injuries, Arthritis and Trigger Finger. Keeping the Hand and Upper Extremity Healthy. https://www.hss.edu/conditions_hand-problems-common-injuries-arthritis-trigger-finger.asp, accessed Mar 31, 2023.
- Pompeu Y, Aristega Almeida B, Kunze K, Altman E, Fufa DT. Current Concepts in the Management of Advanced Trigger Finger: A Critical Analysis Review. JBJS Rev. 2021 Sep 9;9(9). doi: 10.2106/JBJS.RVW.21.00006. PMID: 35417430.
- Wessel LE, Gu A, Asadourian P, Stepan JG, Fufa DT, Osei DA. Incidence of Trigger Finger in Surgically and Nonsurgically Managed Carpal Tunnel Syndrome. J Hand Surg Glob Online. 2022 Nov 24;5(2):164-168. doi: 10.1016/j.jhsg.2022.10.017. PMID: 36974300; PMCID: PMC10039288.
- Yang TC, Fufa D, Huang HK, Huang YC, Chang MC, Wang JP. Percutaneous A1 Pulley Release Combined with Finger Splint for Trigger Finger with Proximal Interphalangeal Joint Flexion Contracture. J Hand Surg Asian Pac Vol. 2019 Sep;24(3):270-275. doi: 10.1142/S2424835519500334. PMID: 31438789.
Updated: 11/2/2023
Reviewed and updated by Duretti Fufa, MD