Periacetabular Osteotomy: An Overview
An interview with HSS surgeon Ernest L. Sink, MD
What is a periacetabular osteotomy?
A periacetabular osteotomy (PAO) is a surgical treatment for hip dysplasia that is caused by a deformity in the acetabulum, the curved portion of the pelvis that forms the socket of the hip joint. Symptoms of this condition – which may be present from birth, but may only become evident in adolescence or adulthood – generally include hip pain and restricted mobility.
Review of hip dysplasia
In the healthy hip, the upper end of the femur (thigh bone) meets the acetabulum in the pelvis, and the two fit together like a ball and socket, in which the “ball” (the femoral head moves freely in the hip socket.[Figure 1.]
Figure 1. Anatomy of a Normal Hip (Image by Smith & Nephew, via Wikimedia Commons)
For some people, hip dysplasia results when the acetabulum does not develop fully, making it too shallow or otherwise misaligned to adequately contain and support the femoral head. Owing to this misalignment, over time the cartilage and labrum (a soft tissue rim made of fibrous cartilage, which lines the hip socket) can end up bearing the brunt of forces that should be distributed throughout the hip. Left untreated, hip dysplasia can result in early degenerative changes – the wearing down of articular cartilage that covers the hip joint surfaces. These changes mark the beginnings of osteoarthritis, in which the protective labrum and articular cartilage wear away, and bone rubs against bone, leading to pain and restricted mobility. Hip dysplasia is one of the common causes of hip pain and arthritis in patients less than 50 years of age.
Hip dysplasia occurs more frequently in women than in men, explains Ernest L. Sink, Associate Attending Orthopedic Surgeon and Co-Director of the Center for Hip Preservation at HSS. Treatment for hip dysplasia ranges from symptomatic relief to surgical correction. In older patients (age 50 and above) with advanced osteoarthritis, total hip replacement may eventually be the best option to alleviate pain and restore mobility. But in younger patients (age 40 and under) in whom joint surface articular cartilage damage has not yet become advanced, a periacetabular osteotomy – in which the surgeon reorients the acetabulum over the femoral head – can offer both symptomatic relief and allow for preservation of the natural hip joint. For patients in their 40s, the most effective treatment is dependent upon the level of hip arthritis.
Diagnosis and presurgical imaging of hip dysplasia
In addition to a thorough physical exam and patient history, orthopedists use X-rays, magnetic resonance imaging (MRI) and, in some cases, three-dimensional CT scans to confirm a diagnosis of hip dysplasia. The highly sophisticated MRI techniques available at HSS are particularly helpful in providing images that show a clear distinction between bone and cartilage, and in pinpointing the extent of damage to the labrum and other soft tissues, if present.
Imaging can also reveal version deformities in the acetabulum, in which the acetabulum tilts too far forward (anteversion) or too far backward (retroversion).
In addition to serving as a diagnostic tool, Dr. Sink and his colleagues also use the three-dimensional CT scans to help plan in advance for anatomical variations in the pelvis they may encounter during surgery. In summary, the diagnosis of hip dysplasia and hip joint stability can be challenging, and it requires careful evaluation of the patient’s symptoms, physical exam and X-rays.
How is hip dysplasia treated?
Nonsurgical treatments
At HSS, many patients with more mild forms of hip dysplasia undergo a trial of nonsurgical treatment with corticosteroid injections and physical therapy. When this approach is successful, the patient is followed with a series of MRIs in order to make sure that there is no progression of damage in the joint. For patients with long histories of symptoms or more severe forms of dysplasia, operative correction is usually recommended at the outset, as long as the extent of hip joint arthritis is not too advanced or severe.
Surgical treatment
If non-operative measures are not successful in patients with mild dysplasia, a PAO may be considered for patients who have reached skeletal maturity with a malalignment of the acetabulum but do not have advanced osteoarthritis. It is not uncommon to recommend a PAO in patients with mild forms of dysplasia when other surgeries have failed, such as a hip arthroscopy, which may repair the labrum but does not correct the underlying dysplasia. The decision to proceed to PAO surgery must take into account the patient’s age and lifestyle. “It’s also important to discuss the patient’s individual goals and expectations,” notes Dr. Sink.
In a periacetabular osteotomy, the surgeon makes a series of cuts to the bone to reposition the acetabulum in the pelvis, in order to restore a more normal hip joint anatomy. Screws are then placed in the bones to stabilize this position. During the healing process, new bone forms across the cut surfaces to secure the repositioned acetabulum in the pelvis, establishing proper alignment of the hip joint ball and socket.[Figures 2. and 3.]
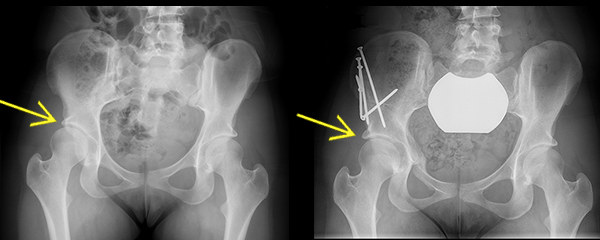
Figure 3. Anterior to posterior X-ray images, before and after a PAO. Left X-ray shows dysplasia of the right hip; the acetabulum is underdeveloped and provides incomplete coverage of the femoral head. Right X-ray shows complete healing of a periacetabular osteotomy, with improved coverage of the femoral head by the acetabulum.
In up to 10% of patients with hip dysplasia a femoral osteotomy may also be necessary to correct malalignment of the upper part (the head and neck) of the femur. Hip arthroscopy may also be performed along with a PAO in selected patients (for example, to repair a damaged labrum).
Throughout the surgery, X-ray guidance is used and the nerves and muscles that surround and support the hip joint are carefully protected.
What is the recovery time of a periacetablular osteotomy?
At HSS, patients who undergo PAO are hospitalized for 2 to 4 days. Physical therapy and instructions on weight-bearing guidelines are initiated before discharge, and crutches must be used for 6 to 8 weeks. Most individuals return to school or work after three months and can resume athletics between 6 to 12 months. If dysplasia affects both hips, the surgeries are performed 4 to 6 months apart.
Periacetabular osteotomy was first developed under the direction of Reinhold Ganz, MD, professor emeritus at the University of Bern in Switzerland. Although the procedure has become more widely used around the world, the HSS Center for Hip Preservation is one of a limited number of centers in the United States where a high volume of these procedures are performed.
In appropriately screened patients who have not developed significant hip joint arthritis, PAOs yield very good results, even up to 20 to 25 years after the procedure.[1] “Performed by an experienced orthopedic surgeon, PAO has a good safety profile and produces predictable results,” says Dr. Sink. “If you are considering undergoing a PAO, it’s important to go to a center where the surgeon evaluates a high volume of young hip patients and the team is very familiar with the PAO and other hip preservations surgeries.”
Reference
1. Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008; 466:1633-1644
Posted: 2/18/2016
Written by Nancy Novick
Authors
Chief, Hip Preservation Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery