Hip Replacement
Hip replacement is a highly successful surgery in which portions of the hip joint are replaced with prostheses (implants). Hospital for Special Surgery (HSS) in New York City performs more hip replacements than any other hospital in the United States. It is ranked the #1 hospital for orthopedics in the United States by U.S. News and World Report as well as the #1 orthopedic hospital in the world in Newsweek's "World's Best Specialized Hospitals."

What is hip replacement surgery?
Hip replacement is the removal and replacement of portions of the pelvis and femur (thighbone) that form your hip joint. It is performed primarily to relieve hip pain and stiffness caused by hip arthritis.
This procedure is also sometimes used to treat injuries such as a broken or improperly growing hip, and for other conditions. (Find a hip replacement specialist at HSS.)
How do you know if you need a hip replacement?
If you have these arthritis symptoms, you should consider a hip replacement:
- severe hip pain that is not relieved by medication and that interferes with your work, sleep or everyday activity
- hip stiffness that restricts motion and makes it difficult to walk
To learn more, read Here’s What to Know if You Think You Need a Hip Replacement.
Hip anatomy
The hip is a ball-and-socket joint. The ball, at the top of your femur (thighbone) is called the femoral head. The socket, called the acetabulum, is a part of your pelvis. The ball moves in the socket, allowing your leg to rotate and move forward, backward and sideways.
In a healthy hip, soft-tissue called cartilage covers the ball and the socket to help them glide together smoothly. If this cartilage gets worn down or damaged, the bones scrape together and become rough. This condition, osteoarthritis, causes pain and restricts motion. An arthritic hip can make it painful to walk or even to get in or out of a chair. If you have been diagnosed with hip arthritis, you may not need surgery. Nonsteroidal anti-inflammatory drugs (NSAIDs) and/or physical therapy may provide relief. But, if these efforts do not relieve symptoms, you should consult an orthopedic surgeon.
What are the different types of hip replacement surgery?
The three major types of hip replacement are:
- total hip replacement (most common)
- partial hip replacement
- hip resurfacing
The most common type of hip replacement surgery is called a total hip replacement (also called total hip arthroplasty). In this surgery, worn-out or damaged sections of your hip are replaced with artificial implants. The socket is replaced with a durable plastic cup, which may or may not also include a titanium metal shell. Your femoral head will be removed and replaced with a ball made from ceramic or a metal alloy. The new ball is attached to a metal stem that is inserted into the top of your femur. (Learn more about types of hip implants.)
Healthy hip
Arthritic hip
Replaced hip
Two other types of hip replacement surgeries are each generally appropriate for patients of specific age groups and activity levels:
- Partial hip replacement (also called hemiarthroplasty) involves replacing only one side of the hip joint – the femoral head – instead of both sides as in total hip replacement. This procedure is most commonly done in older patients who have fractured their hip.
- Hip resurfacing of the femoral head and socket is most commonly done in younger, active patients.

X-ray of a total hip replacement showing the ball, socket and stem implants
Hip replacement surgical methods
There are two major surgical approach methods for performing a total hip replacement:
- the posterior approach (more common)
- the anterior approach (sometimes called the "mini-anterior approach" or "muscle-sparing hip replacement")
To begin the operation, the hip replacement surgeon will make incisions on either the back (posterior) or front (anterior) of the hip. Both approaches offer pain relief and improvement in walking and movement within weeks of surgery. In some instances, the orthopedic surgeon may choose to employ robotic technologies during the surgery. (Find an HSS surgeon who performs robotic-assisted hip replacement surgery.)
Total hip replacement animation: Posterior approach
How should I prepare for hip replacement surgery?
There are certain steps patients can take both before and after surgery to improve recovery time and results. It is important to follow the instructions and guidance provided by your orthopedic surgeon, medical team and rehabilitation therapist. Visit Preparing for Your Surgery to get information on preoperative hip replacement classes and patient education materials about joint replacement surgery.
Can hip replacement be done as an outpatient?
Most patients will stay in the hospital one or two nights after surgery. Some patients may be able have same-day hip replacement and return home after an outpatient procedure.
Learn more about same-day hip replacement by reading Outpatient Hip Replacement Surgery: Frequently Asked Questions.
How long does hip replacement surgery take?
Total hip replacement surgery takes about one and a half hours. Most patients also stay in the hospital for one or two days after the procedure.
How long does it take to recover from a hip replacement?
Your rehabilitation will begin within 24 hours after surgery. Most hip replacement patients progress to walking with a cane, walker or crutches within a day or two after surgery. As the days progress, you will increase the distance and frequency of walking. Full recovery generally takes anywhere from two to eight weeks, depending on the patient's general health and other factors.
If you have total hip replacement surgery at HSS:
- Your recovery will begin directly following surgery in the Post-Anesthesia Care Unit (PACU), where your medical team will manage your pain and monitor your vital signs.
- Once the anesthesiologist is satisfied with your condition, you will be moved to an inpatient recovery room to monitor your progress. Appropriate candidates for outpatient surgery will be discharged when medically appropriate.
- You will most likely have a dressing and tube on your hip for drainage, which should be removed the day after surgery.
- The pain management team will assess your medication and use a multifaceted approach to ensure comfort and mobility during the rehabilitation process.
- You will begin rehabilitation with a physical therapist within 24 hours. Your therapist will help you sit up, get in and out of bed, and practice walking and climbing stairs using a walker, cane or sometimes crutches.
- You will then continue physical therapy outside the hospital for six to eight weeks. After that period, most patients are able to do everyday activities and return to playing sports.
Learn more in our series of articles about hip replacement recovery.
Can I have both hips replaced at the same time?
Yes, healthy patients younger than 75 years old who have no history of cardiopulmonary disease may be able to have both hips replaced at once. In some cases, however, it may be better to stage the surgeries.
What are the risks in hip replacement surgery?
Total hip replacement is a major surgery. It is very safe, but every surgery has risks. Risks in a hip replacement include blood clots in the leg or pelvis, or a hip dislocation. But the most serious risk, however, is of an infection. You should ask your surgeon what the surgical infection rate is for hip replacements at the hospital or facility where you will have your surgery.
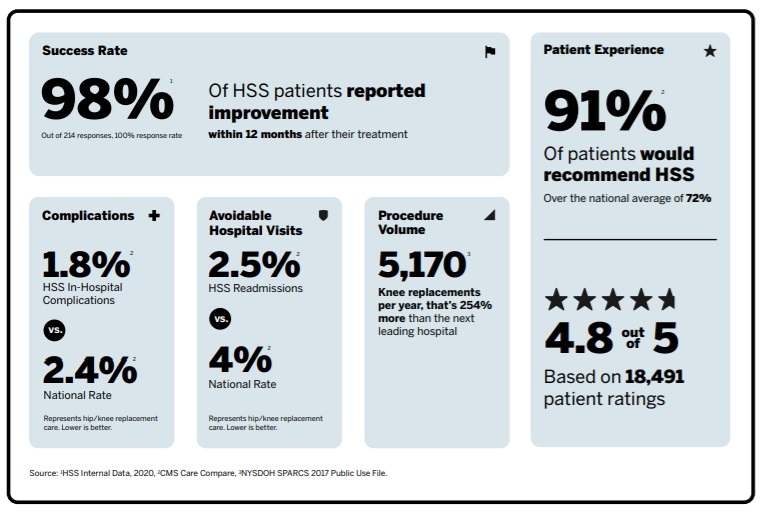
HSS has one of the lowest rates of infection for hip replacement surgery, as well as a significantly lower rate of readmission compared to the national average. In 2015, The New York State Department of Health reported that out of more than 160 hospitals in New York that did hip replacements in 2014, only Hospital for Special Surgery had a hip replacement surgery site infection (SSI) rate that was "significantly lower than the state average" for that year, and that those infection rates at HSS had been significantly lower than the state average in each of the seven years between 2008-2014.
Other risks include blood clots in the leg or pelvis, and accidental hip dislocation during or after recovery. Hospital for Special Surgery performs better than the national average in preventing blood clots after surgery.
What are hip implants made of?
There are three separate implants: the stem, the ball and the socket.
- The stem, made out of metal (usually titanium or cobalt-chrome) is inserted into your natural thighbone.
- The ball is usually made out of polished metal or ceramic, and fits on top of the stem.
- The socket is usually a combination of a plastic liner and a cobalt-chrome or titanium backing.
Will my new hip set off the metal detector at the airport?
Today's sensitive screening machines will detect the implant but can also effectively identify it. The machine operator will know that it is an implant rather than an unauthorized metal object contained outside the body.
It is still helpful to tell airport security that you have had a hip replacement before entering the screening machine. You may also ask your doctor's office if they can provide a card that identifies that you have received a hip implant that contains metal.
How long do hip implants last?
Generally speaking, a hip replacement prosthesis should remain effective for between 10 and 20 years, and some can last even longer.
Results vary according to the type of implant and the age of the patient. In a 2008 study of more than 50,000 patients who had THR surgery at age 55 or older, between 71% and 94% still had well-working implants after 15 years.
When a hip implant does need to be replaced because it has loosened or worn out over time, this requires what is called hip revision surgery.
How soon after surgery can I resume driving?
Most patients can resume driving by six weeks after surgery.
What should I look for in a hip replacement surgeon?
When looking for an orthopedic surgeon to perform your hip replacement surgeon, it’s important to do your research and check the surgeon’s credentials, experience and reputation. It is also important to research the hospital or facility where you will have your operation, as well as its supporting staff, such as the anesthesiologists.
How successful is total hip replacement surgery?
In general, the success rate for hip replacement surgery is high: About 95% of patients experience relief from hip pain and 90% to 95% of implants remain viable 10 years after surgery, while 80% to 85% remain so after 20 years. In a study, HSS interviewed patients to learn about their progress. Two years after their surgeries, 99.4% of patients said they had relief from pain, 98.8% said their ability to move was improved, and 97.8% said their quality of life was better because of their surgery.
Should an implant wear or loosen, revision to a new hip replacement is possible.
Below, explore detailed articles and other content on this topic, or find a hip replacement surgeon at HSS to suit your specific condition, location and insurance.
Why you should choose HSS for hip replacement
Hip replacement is a surgery focused on reducing pain and getting you back to the activities you love. But not all hospitals achieve the same results. Some are more reliable than others. With the help of the HSS Hospital Reliability Scorecard, you can make sure you're asking the critical questions to find the hospital that's right for you. Understanding these data points will help you make the best decision for your care: See hospital reliability data
Hip replacement surgery overview articles
Get more detailed information on different types of hip replacement surgeries, implants and related topics.
- Here’s What to Know if You Think You Need a Hip Replacement
- Outpatient Hip Replacement Surgery: Frequently Asked Questions
- Anterior Approach Hip Replacement: An Overview
- Revision Total Hip Replacement: An Overview
- New Technology in Hip and Knee Replacement Surgery at HSS
- Dual Mobility Hip Replacement: An Attractive Option for Younger Patients
Hip replacement recovery articles
Learn more about the days and weeks after hip replacement, and getting back to your favorite activities.
Related articles from HSS Move Better Feel Better
HSS Move Better Feel Better features tips on health, mind-body issues, fitness, and injury prevention for adults and children.
Hip Replacement Success Stories
References
- González Della Valle A, Sharrock N, Barlow M, Caceres L, Go G, Salvati EA. The modern, hybrid total hip arthroplasty for primary osteoarthritis at the Hospital for Special Surgery. Bone Joint J. 2016 Jan;98-B(1 Suppl A):54-9. doi: 10.1302/0301-620X.98B1.36409. PMID: 26733642.
- Koltsov JCB, Marx RG, Bachner E, McLawhorn AS, Lyman S. Risk-Based Hospital and Surgeon-Volume Categories for Total Hip Arthroplasty. J Bone Joint Surg Am. 2018;100(14):1203-1208. doi:10.2106/JBJS.17.00967.
- Kunze KN, Bovonratwet P, Polce EM, Paul K, Sculco PK. Comparison of Surgical Time, Short-term Adverse Events, and Implant Placement Accuracy Between Manual, Robotic-assisted, and Computer-navigated Total Hip Arthroplasty: A Network Meta-analysis of Randomized Controlled Trials. J Am Acad Orthop Surg Glob Res Rev. 2022 Apr 1;6(4):e21.00200. doi: 10.5435/JAAOSGlobal-D-21-00200. PMID: 35472191.
- Memtsoudis SG, Cozowicz C, Bekeris J, Bekere D, Liu J, Soffin EM, Mariano ER, Johnson RL, Go G, Hargett MJ, Lee BH, Wendel P, Brouillette M, Kim SJ, Baaklini L, Wetmore DS, Hong G, Goto R, Jivanelli B, Athanassoglou V, Argyra E, Barrington MJ, Borgeat A, De Andres J, El-Boghdadly K, Elkassabany NM, Gautier P, Gerner P, Gonzalez Della Valle A, Goytizolo E, Guo Z, Hogg R, Kehlet H, Kessler P, Kopp S, Lavand'homme P, Macfarlane A, MacLean C, Mantilla C, McIsaac D, McLawhorn A, Neal JM, Parks M, Parvizi J, Peng P, Pichler L, Poeran J, Poultsides L, Schwenk ES, Sites BD, Stundner O, Sun EC, Viscusi E, Votta-Velis EG, Wu CL, YaDeau J, Sharrock NE. Peripheral nerve block anesthesia/analgesia for patients undergoing primary hip and knee arthroplasty: recommendations from the International Consensus on Anesthesia-Related Outcomes after Surgery (ICAROS) group based on a systematic review and meta-analysis of current literature. Reg Anesth Pain Med. 2021 Nov;46(11):971-985. doi: 10.1136/rapm-2021-102750. Epub 2021 Aug 25. PMID: 34433647.
- Robinson J, Bas M, Deyer T, Cooper HJ, Hepinstall M, Ranawat A, Rodriguez JA. Muscle recovery after total hip arthroplasty: prospective MRI comparison of anterior and posterior approaches. Hip Int. 2022 Oct 3:11207000221114456. doi: 10.1177/11207000221114456. Epub ahead of print. PMID: 36192819.
- Rodriguez S, Shen TS, Lebrun DG, Della Valle AG, Ast MP, Rodriguez JA. Ambulatory total hip arthroplasty: Causes for failure to launch and associated risk factors. Bone Jt Open. 2022 Sep;3(9):684-691. doi: 10.1302/2633-1462.39.BJO-2022-0106.R1. PMID: 36047458.
- Hospital-Acquired Infections, New York State. New York State Department of Health, Albany, NY. October 2015. https://www.health.ny.gov/statistics/facilities/hospital/hospital_acquired_infections/2014/docs/hospital_acquired_infection.pdf.
- HSS Arthroplasty Registry, 2007-2012. https://www.clinicaltrials.gov/ct2/show/NCT00454506.
- Newsweek's "World's Best Specialized Hospitals 2022."
- NYSDOH SPARCS 2017 Public Use File, https://www.health.ny.gov/statistics/sparcs/access/.
- U.S. News & World Report "Best Hospitals for Orthopedics."
Reviewed and edited by Edward C. Jones, MD, MA.