Applied Biomechanics at Hospital for Special Surgery
Every year in the United States, millions of people with stiff and painful joints seek medical attention for a range of musculoskeletal conditions, most related to trauma or osteoarthritis. Fortunately, many can be treated with conservative methods, including proper conditioning, lifestyle changes, and medication. For others, a variety of surgical procedures, such as ligament and cartilage repair, osteotomy (joint realignment) or joint arthroplasty (replacement) may be necessary to relieve their pain and to allow them to resume their daily activities.
Many treatments used today have emerged from the collaborative efforts of biomechanical engineers and orthopedic surgeons. Beginning in the late 1960s with its creation of the Department of Biomechanics, HSS became one of the pioneers in this important collaboration. "This department was created on the premise that orthopedics and biomechanical engineering go hand-in-hand," says Timothy Wright, PhD, F.M. Kirby Chair of Orthopedic Biomechanics and Director of the current Biomechanics Department. "The musculoskeletal system is basically a mechanical machine that orthopedic surgeons work with all the time."
The department serves a dual purpose at HSS, according to Dr. Wright. HSS surgeons often have ideas for better solutions, for example an improved joint prosthesis – solutions that require engineering expertise – and can work directly with a team of engineers with years of experience working in the field. In addition, the necessary efforts required to bring these ideas to fruition afford the Hospital’s residents and fellows the opportunity to participate in cutting-edge research and development that teaches them about the mechanical consequences of both the conditions they will face and the choices they will make in treating musculoskeletal problems.
This exchange of ideas has expanded to include participation by the manufacturers of orthopedic implants. The practical outcome of these collaborations is new innovations and products that have the potential to significantly improve patients’ lives. The integration with manufacturers and the transfer of technology from HSS to the market through the efforts of the HSS Innovation Institute ensures that technological advances made at HSS can reach patients worldwide.
The development of the Insall-Burstein knee implant in the late 1970s provides an early example of this type of teamwork. John Insall, MD, an orthopedic surgeon, and Albert Burstein, PhD, a biomechanical engineer, built customized knee implants for patients at HSS who required total knee arthroplasty. Based on the success of these implants, they were able to create a generic system of prostheses suited to most patients requiring knee replacement. "The entire system from the major components to the instruments used to implant them were designed and developed in our department," explains Dr. Wright. The Hospital then reached an agreement with major orthopedic device manufacturers, Johnson & Johnson and Zimmer, to produce and market the Insall-Burstein™ knee prosthesis. The concepts incorporated in the Insall-Burstein knee, and the subsequent technologically advanced designs made by HSS surgeons and engineers, have been used worldwide with significant success. In fact, the basic concept of the Insall-Burstein knee is now used in about half of all total knee replacements used worldwide.
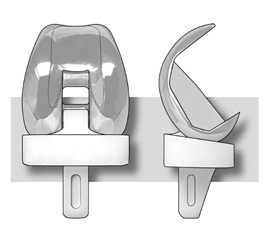
Illustration of the Insall-Burstein knee replacement prothesis
Today, when engineers and surgeons at HSS have an idea for a product, collaboration with a manufacturer begins at a much earlier stage. "It’s a win-win situation," explains Dr. Wright. "The Hospital and the company bring different and complementary resources to the process." The Hospital can rely on the manufacturer to provide important additional engineering steps (for example, expertise in manufacturing and tolerances), which eliminates the need to have those resources in-house.
Since the development of the Insall-Burstein design, engineers and surgeons at HSS have pursued continual improvement in the performance of total knee replacements. Newer designs provide for greater motion of the knee, are more resistant to wear, and now provide more levels of constraint so that the implant can better restore joint stability. The most recent efforts have been to design knee components that can be fixed to the surrounding bones biologically. These components have porous metallic surfaces that, when placed rigidly next to the bone, elicit bone tissue to invade the pores, rigidly locking the implant in place. The result is a long-lasting bond that eliminates the need for bone cement, a polymeric grout used to secure most conventional knee components.

A prototype cementless, porous tibial component for knee replacement
The development of modern porous components for biologic fixation is being greatly enhanced by the growing role of 3D printing (also called additive manufacturing) in making implant components for joint replacement. “This exciting technology opens up the design space,” says Dr. Wright, “because if you can think about a structure in three dimensions you can build it with 3D printing, whereas you may not be able to make it with more conventional manufacturing techniques like machining parts from a solid block of metal.”
The ability to tailor the porosity provides the opportunity to maximize the interaction between the implant and the bone, thus optimizing the conditions for bone ingrowth. Engineers in the Biomechanics Department have worked with their surgeon colleagues to develop sophisticated computer models that are helping to determine these optimal solutions. The result of these efforts are porous implants that mimic local bone structures and that can, depending on the design requirement, range from totally solid to completely porous.
The unique collaborations that result from 3D printing follow the same criteria that any design project must meet at HSS. The most important, according to Dr. Wright, is the need for a surgeon "champion," a clinical expert with thorough understanding of the problem and who has an innovative idea – one with the promise to yield a product that will provide substantial benefit to patients. Over the years, this approach has led to the design of implants for hip, knee, shoulder, elbow, wrist, thumb, and ankle replacements.
Another recent example of these efforts is a hip replacement system for the pediatric population. Unfortunately, young people, too, suffer from joint diseases for which the only treatment to restore function and eliminate pain is a joint replacement. HSS has a long history of treating these patients. Often, they require custom designs because of the distorted anatomy that accompanies their condition. But the extensive experience HSS has in hip replacements for young patients, together with improvements in implant design, afforded the development of a system that can accommodate the needs of this special class of patients.
“Appropriately sized implants are an unmet need for the pediatric population,” says Mark P. Figgie, MD, Chief Emeritus of the Surgical Arthritis Service and an Attending Orthopedic Surgeon at HSS. “In many cases, the adolescent requires a patient-specific implant due to the unusual deformity and small size. These implants are challenging to design and expensive to manufacture, so our goal is to design a system that will eliminate their need in the majority of these cases.
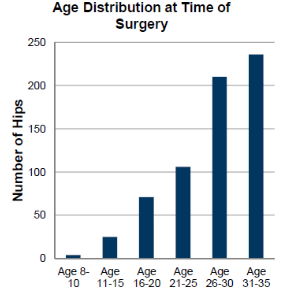
Since 1986, more than 800 hip replacements have been performed by HSS surgeons in patients under the age of 35. Courtesy of Dr. Mark Figgie.
In all areas of research and development, the team is guided by the goal of producing a product that will improve clinical outcomes. Of their collaboration with manufacturers Dr. Wright says, "We are always looking for ideas that are going to benefit our patients. And commercial entities are always looking to HSS as a source of innovative solutions that can impact the broad orthopedic community."
Updated: 5/4/2020
*Summary Prepared by Nancy Novick
Authors
Senior Scientist, Hospital for Special Surgery
F.M. Kirby Chair, Orthopaedic Biomechanics
Chief Emeritus, Surgical Arthritis Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery



