Herniated Disc (Ruptured or Slipped Disc)
Intervertebral discs are rubbery cushions between the segmental bones of the spine (vertebrae). They act as shock absorbers and provide the normal flexibility of the spinal column. Each disc’s normal location is directly adjacent to the spinal nerves.
What is a herniated disc?
A herniated disc (also known as a disc herniation and sometimes called a "slipped disc") occurs when a piece of a spinal disc bulges or ruptures and slips out of place, squeezing a spinal nerve. This may cause leg pain, leg weakness, leg numbness, cauda equina syndrome, and/or low back pain.
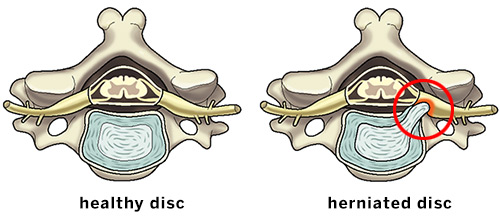
Illustrations of the axial (overhead) view of a healthy cervical disc and a herniation putting pressure on a spinal nerve.
Why does a disc herniate?
Unlike most other parts of the body, lumbar discs begin to deteriorate (degenerate) at a young age. Many patients in their twenties will have disc degeneration on X-rays or MRI and virtually 100% of elderly people have multiple degenerated discs.
As discs degenerate they lose their water content and elasticity, and the retaining wall around the disc (annulus) begins to fissure or tear. Pieces of the deteriorating disc can then protrude out (herniate) through the leaking annulus. As the disc degenerates, low back pain may result. If herniated disc fragments compress a spinal nerve, it may result in leg pain, weakness, and/or numbness.
Discs often herniate without any unusual traumatic event, but in some cases there may be contributing factors such as excessive weight, poor posture, heavy lifting, or trauma.
Which spinal discs herniate most frequently?
Although a herniation can occur in any section of the spine, herniated discs in the lumbar (low back) and cervical (neck) spine are the most common. Symptoms may include low back or neck pain, along with pain radiating into the leg (sciatica) or arm, along with weakness and/or numbness. A herniated disc in the neck can cause a condition known as cervical radiculopathy.
What are the symptoms of a herniated disc?
The most typical symptom of a disc herniation is pain that radiates from the low back down into the leg (sciatica). In addition to leg pain, the leg may also be weak or numb. One or both legs may be affected. Rarely, bowel or bladder function may be affected. Most patients with disc herniation also experience low back pain.
How is a herniated disc diagnosed?
Only a medical professional can diagnose a disc herniation. A thorough medical history and physical examination can point to the possibility of a disc herniation. The diagnosis can be confirmed by special tests such as MRI and/or CT myelography (myelogram).
What is the best treatment for a herniated disc?
Most lumbar disc herniations go away on their own without any treatment. For painful herniations that persist, treatment begins with the least invasive options, such as anti-inflammatory medications and physical therapy. If symptoms continue, epidural steroid injections may be recommended. If nonsurgical methods do not provide relief, lumbar microdiscectomy surgery (microdecompression) typically provides excellent relief.
One notable exception to the use of surgery as the last treatment in lumbar disc herniation is in those patients who have significant weakness in leg muscles, in which case early surgery may be recommended in order to minimize the possibility of permanent nerve damage and persistent leg weakness.
Explore the content below to learn more or find a find a doctor at HSS who treats disc herniations.

Herniated disc articles
Read more about back pain and slipped disc conditions.
Herniated disc treatment articles
Learn about different forms of surgical and nonsurgical treatment of herniated discs.
- ALIF Surgery: Anterior Lumbar Interbody Fusion
- Epidural Steroid Injections: Frequently Asked Questions
- Spinal Cord Stimulator – A Compelling Treatment Technique for Chronic Pain
- Microdiscectomy: Surgical Treatment for a Herniated Disc
- ACDF Surgery: Anterior Cervical Discectomy and Fusion
- Spine Surgery: Minimally Invasive Lumbar Discectomy / Percutaneous Disc Removal (PDR)
- Spine Surgery: Posterior Cervical Laminotomy
- Lumbar Fusion
- TLIF Surgery: Transforaminal Lumbar Interbody Fusion
- PLIF Surgery: Posterior Lumbar Interbody Fusion
- Minimally Invasive Lower Back Surgery for Disc Degeneration: The Anterolateral (Side) Approach
Articles on related topics
Herniated Disc (Ruptured or Slipped Disc) Success Stories
In the news


