Michael L. Parks, MD, FAAOS, Named Second Vice President of the American Academy of Orthopaedic Surgeons Board of Directors.
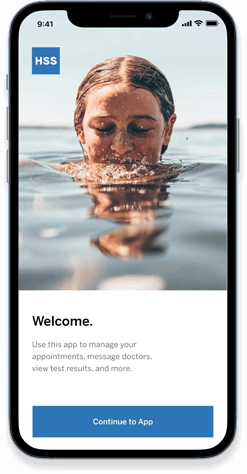
Choose better. Move better.
Schedule an in-person appointment with a physical therapist
Physical TherapyWe offer convenient same-day options for orthopedic care
Get Immediate CareWe're proud to share the remarkable accomplishments that have contributed to our hospital's reputation for excellence.
See all our rankingsWe receive consistently high ratings from our patients for the quality of our doctors and our hospital. More than 3,000 have shared their experience in their own words. Search stories by condition, doctor, hometown, or even favorite activity.
Read their storiesFrom diagnosis to surgery, our top ranked orthopedic and rheumatology specialists can explain your treatment options and provide the care you need.
Learn why you should choose HSS
See our top rankings
Compare hospital reliability