ACDF Surgery: Anterior Cervical Discectomy and Fusion
Surgery to treat spinal cord or nerve pressure from myelopathy, herniated discs and other conditions
Anterior cervical discectomy with fusion (ACDF) is a combination spinal decompression and spinal fusion surgery used to treat herniated discs, compressed nerves or other conditions in the neck.

A disc herniates when the outer portion of the disc ruptures and some of the softer disc nucleus material squeezes out. The herniated disc pushes against the spinal cord or spinal nerves and tends to cause pain in the neck or arms. This procedure removes the ruptured disc to alleviate pressure on the nerves or spinal cord, which usually relieves the pain.
What is ACDF surgery?
Anterior cervical discectomy and fusion (ACDF) is a common treatment of disc herniations, myelopathy and other problems arising in the cervical spine (the bones of the neck between the base of the skull and the top of the chest).
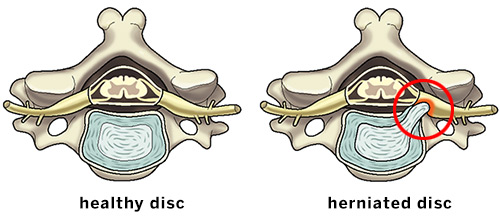
Illustrations of the axial (overhead) view of a healthy disc and a herniated disc putting pressure on a spinal nerve.
This minimally invasive surgery involves a discectomy (removal of the soft disc between the vertebra) and the replacement of this soft tissue with graft material (the patient’s own bone, donor bone, or synthetic material). This stimulates the healing of the bones together, referred to as fusion. (Find an HSS surgeon who performs ACDF surgery.)
Cervical spine anatomy and the minimally invasive approach
An introduction to the relevant anatomy of the front (anterior) of the neck, including the trachea, esophagus, cervical spine and surrounding tissues, is useful to help explain the minimally invasive approach of the ACDF procedure.
In the middle of the neck lies the trachea (windpipe) and esophagus (the muscular pipe that allows you to swallow foods and drinks). These lie just in front of the cervical spine. On either side of these structures are a collection of muscles and blood vessels, most importantly the sternocleidomastoid (SCM – the muscle that allows you to turn your head from side to side) and the carotid arteries (which carry blood from the heart up to the brain). By delicately separating these structures, a spine surgeon has easy access to the cervical spine through small incisions with minimal dissection.
Who is a good candidate for ACDF surgery?
ACDF surgery is an excellent surgical option for patients who are experiencing nerve pain in the neck that radiates down to their shoulder and arms (known as cervical radiculopathy or brachialgia) or for patients who have cervical spinal cord compression (known as cervical myelopathy).
In both cases, the removal of the disc or bone spur which is causing compression on the nerve or spinal cord can provide fast relief of pain symptoms and prevent worsening of conditions related to spinal cord compression. Even patients who have had prior head and neck surgeries can be good candidates for ACDF – please consult with your orthopedic surgeon.
What does ACDF surgery treat?
ACDF can be used to treat a number of cervical spine issues. The most common reason for ACDF is to treat cervical radiculopathy (nerve pain that radiates from the neck down to the shoulder or arms). This can be caused by cervical disc herniation (where a piece of the soft disc presses on the nerve) or by worsening arthritis of neck joints, which produces bone spurs (known as cervical spondylosis). These same processes can sometimes cause compression of the spinal cord itself, which is known as myelopathy. Less commonly, ACDF can treat cervical spine fractures or may be necessary after separate treatments for a spinal infection or spinal tumor.
Is ACDF surgery painful?
ACDF is a minimally invasive procedure, meaning less soft tissue can be dissected to achieve surgery success than in conventional, open procedures. After ACDF surgery, some patients may experience throat soreness or a hoarse voice, each of which will resolve quickly after surgery. Patients may likewise experience temporary discomfort when swallowing. In rare instances, some patients may have difficulty swallowing fully, known as dysphagia, which can be treated.
How is anterior cervical discectomy and fusion performed?
The procedure is performed at one or more disc levels in the spine simultaneously through an incision in the front of the neck. To perform ACDF surgery, general anesthesia is required, meaning patients are completely asleep during the procedure and a breathing tube is placed to assist with breathing during the procedure.
A small surgical incision is made over the front of the neck, generally off to the side in a location where scarring will not be clearly visible. The sternocleidomastoid (SCM) muscle and carotid arteries are separated from the trachea and esophagus, and each is protected using specialized tools called retractors (either tubular or rectangular) throughout the procedure. The soft disc is then carefully removed, along with any herniated pieces or bone spurs that are causing compression on the nerves.
The area is then thoroughly cleaned and graft material (the patient’s own bone, donor bone, or synthetic material) is inserted where the soft disc used to be. After the graft is placed and checked a thin, metallic or plastic plate is attached to the bone to secure the graft in place. After the procedure, patients generally wear a collar to provide neck support for a short period of time according to surgeon’s plan.
Animation: Anterior cervical discectomy with fusion (ACDF)
This animation provides an inside look into an instrumented anterior cervical discectomy with fusion (ACDF), in which a portion of a ruptured spinal disc in the neck is removed to remove pressure on nerves caused by a herniated disc. A bone graft is usually inserted with instrumentation to keep the disc space at a normal height and fuse the vertebrae above and below the removed disc.
How long does ACDF surgery take?
ACDF surgery is a relatively fast procedure because of the minimally invasive nature, however surgical times can vary depending on the number of spinal levels (individual vertebrae) being addressed at a time. Patients can expect about an hour to an hour-and-a half of actual surgical time to perform a single-level ACDF. Time spent in the operating room is slightly longer, which includes time to induce anesthesia, position the patient on the operating table, and safely awaken and transfer the patient once the surgery is complete.
What is the recovery time for ACDF surgery?
Recovery time is rapid following ACDF. In some cases, such as single-level surgery, patients may be able to go home the same day – this should be discussed with the surgeon beforehand. In most other cases, people should expect to stay one night in the hospital. Patients are then able to recover at home and participate in normal activities of daily life immediately (such as bathing, dressing, eating, and light walking). Patients should discuss postoperative recovery with their surgeon – in most cases low-impact aerobic exercise such as walking, elliptical exercise, and stationary bicycling can be done immediately. In the span of 6 to 12 weeks, most patients will be enrolled in a formal physical therapy program to work on neck range-of motion-exercises and gradually returning to unrestricted activity.
How successful is ACDF surgery?
ACDF is highly successful in treating appropriate cervical spine conditions.
What risks or complications can occur with ACDF surgery?
In general, there are risks for any surgical procedure, including risk of infection, bleeding, and damage to nearby structures. Thankfully, in ACDF surgery, the risks of infection are extremely low – less than one in 1,000 cases. Instances of bleeding, which require careful monitoring or a return to the operating room, are also exceedingly rare particularly because of the exceptional, minimally invasive techniques employed to perform this procedure. Lastly, there are several structures in the region of the surgery that will be monitored for injury, such as the esophagus.
Most importantly the surgery takes place at the level of the spinal cord – during surgery there is real time monitoring of spinal cord health using electrical stimulation which can alert the surgeon to any issues. Meticulous care by the anesthesiologist is employed to maintain cord health. The muscular esophagus, which carries what we eat and drink to the stomach is also in the surgical field.
Occasionally, patients will experience a sore throat when swallowing or a “lump” in their throat sensation due to the surgical exposure and breathing tube. This improves rapidly as swelling in the area decreases. In 1% of cases patients may experience a sense of “heaviness” or weakness in their upper arm or deltoid muscles. This is due to a process called neuropraxia or stretching of the nerve. As the surgery decompresses and relieves pressure on the nerves, this rare phenomenon can occur at the fifth cervical root. This neuropraxia resolves with time. Because ACDF is performed in the region of the neck and at the level of the spinal cord, clinicians at HSS take postoperative care very seriously. All staff involved in patient care are highly trained to recognize problems and provide immediate care.
Updated: 8/1/2022
Authors
Assistant Attending Orthopedic Surgeon, Hospital for Special Surgery
Assistant Professor of Orthopedic Surgery, Weill Cornell Medical College
