Center for Brachial Plexus and Traumatic Nerve Injury
Nationally Recognized Resource
The Center for Brachial Plexus and Traumatic Nerve Injury at Hospital for Special Surgery is a nationally recognized resource for men and women of all ages, providing diagnostic and reconstructive options for patients with injuries to or dysfunction of the peripheral nerve and brachial plexus.
Using a multidisciplinary approach, our Center utilizes the expertise of a wide range of health care professionals including orthopedic surgeons, physiatrists, neurologists, radiologists, psychiatrists, rheumatologists, pain management specialists, social workers, physical therapists, and anesthesiologists so patients can benefit from a coordinated treatment experience.
Our specialists coordinate the clinical and research capabilities of HSS to continually provide state-of-the-art diagnostic and reconstructive options for patients with these devastating injuries.
One of the goals for our Center is to be a resource for hand and upper extremity medical professionals around the world.
Advances in nerve surgery have improved movement and function, while simultaneously diminishing pain.
What Is the Brachial Plexus?
The brachial plexus is a system of nerves that conduct signals to the shoulder, arm and hand. These nerves exit from the spinal cord in the neck to direct the movement and touch sensations of the upper arm.
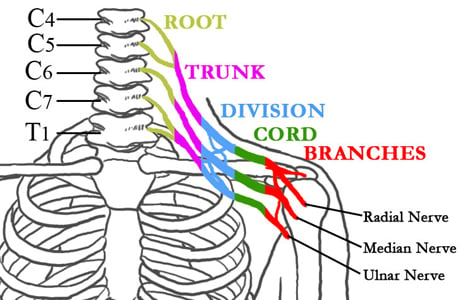
Figure 1: The nerves of the Brachial Plexus in relation to the spine, ribcage, shoulder, and arm.
What Is a Brachial Plexus Injury?
The basic types of brachial plexus injury are:
- constriction - being pinched or squeezed
- neuropraxia - being pulled, strained or stretched
- ruptured - being cut or torn in half
- avulsion - being torn completely away from the spinal cord at the nerve root
Brachial Plexus Injury Symptoms
Brachial plexus injury symptoms felt in the arm and shoulder can include:
- numbness
- weakness
- paralysis
- pain
- loss of feeling
What Causes a Brachial Plexus Injury?
These injuries are caused by high-impact traumas such as:
- vehicle collisions (car or motorcycle accidents)
- industrial accidents
- falls from high height
- being shot with a gun or stabbed
A traumatic injury of the brachial plexus can have devastating consequences, including loss of function and chronic pain for an otherwise healthy, active patient. Fortunately, new advances in nerve surgery can yield marked improvement in movement and function in the shoulder, elbow and hand while simultaneously diminishing pain.
Early recognition and treatment of this injury, along with the recent advances that have been made in microsurgical reconstruction, have greatly improved outcomes for patients. Injuries for which restoring function would have been impossible only two decades ago are now being treated with nerve reconstruction, increasing the possibility of a return to an active, productive life.
The Center for Brachial Plexus and Traumatic Nerve Injury at HSS leads a multidisciplinary approach to expertly treat injuries of the brachial plexus and peripheral nerves.
Adult and Pediatric Brachial Plexus Injuries
A brachial plexus injury can have a devastating effect on upper limb function. Traumatic brachial plexus injuries, which are most commonly sustained in high-speed motor vehicle accidents or sporting events, are characteristically complete, and affect the sensibility and muscle power of the entire extremity. Read more: Adult and Pediatric Brachial Plexus Injuries
Brachial Plexus Injuries Can Be Devastating
Injuries to the brachial plexus (nerves that conduct signals to the shoulder, arm, and hand) can have devastating consequences, including loss of function and chronic pain. Fortunately, new advances in nerve surgery can yield marked improvement in movement and function of the shoulder, elbow, and hand, while simultaneously diminishing pain. Read more: Brachial Plexus Injuries: New Advances in Treatment
Thoracic Outlet Syndrome
Thoracic outlet syndrome (TOS) is a syndrome that can involve the compression of veins, arteries and/or the brachial plexus nerves. It can cause any combination of:
- pain
- weakness
- numbness
- tingling
- a cold sensation
- general discomfort in one or both arms
Our Brachial Plexus Specialists
The Center’s multidisciplinary team is an important resource for patients seeking comprehensive treatment for brachial plexus and other complex nerve injuries. HSS is nationally ranked No. 1 in orthopedics (for 16 years in a row) and No. 3 in rheumatology by U.S. News & World Report (2025-2026). Our comprehensive team approach utilizes experts in the fields of orthopedics, physiatry, neurology, radiology, pain management, psychiatry, rheumatology, social work, physical therapy, and anesthesiology. Working hand-in-hand with our researchers, our staff is constantly evaluating and improving our surgical techniques and investigating new approaches.
The Center for Brachial Plexus and Traumatic Nerve Injury specialists will coordinate the clinical and research capabilities of HSS to continually seek and provide state-of-the-art diagnostic and reconstructive options for patients.
Surgeons and Physicians






First of Its Kind
Our Center is among the first of its kind to offer a multi-disciplinary approach to brachial plexus and peripheral nerve injury and treatment as well as education and research. Combining the medical expertise of specialists and researchers in the fields of orthopedics, physiatry, neurology, radiology, psychiatry, rheumatology, pain management, social work, physical therapy and anesthesiology, the Center is leading the way in diagnosis and treatment of these devastating conditions while providing patients with the best and most up-to-the minute medical care.
Psychosocial Support for Patients
We recognize that brachial plexus injuries affect patients' lives in more than just a physical way. Our Center social worker meets with patients to provide emotional support as well as education about the commonly experienced impacts on one's life following brachial plexus injury. Examples might include changes in outlook on life, self-esteem, and interactions with others. As research has shown that mood impacts recovery, our aim is to provide a holistic perspective to best support your healing. In addition to providing emotional support and education, our social worker can provide referrals to helpful resources in your community.
Research
Our Center surgeons and scientists collaborate to develop a basic science research program as a means to better understand and modulate peripheral nerve regeneration. Researchers are focusing on new ways and techniques to treat injuries to the brachial plexus and peripheral nerve. In the Motion Analysis Laboratory, we refine novel means to measure functional recovery and measure three-dimensional extremity motion.
Registry
Our clinical registries will incorporate a universal outcomes tool for the upper extremity that is in development at Hospital for Special Surgery. Investigational research on nerve imaging could potentially augment the diagnostic potential of clinicians. The synergy of a multispecialty team will establish an efficient model for cultivating innovative ideas and concepts and bring them from bench to bedside.
Education
This webpage offer detailed descriptions of conditions, treatment options and procedures to provide patients with the information they need to manage their care.
Conditions and Disorders
Avulsion
In brachial plexus injuries, the term avulsion is used to describe a condition where the roots of the nerves are torn away from the spinal cord. Multiple root avulsion is the most common diagnosis in high-energy, traumatic brachial plexus injuries, such as occur in a motorcycle or off-road vehicle accident.
Axillary Nerve Palsy (Deltoid Paralysis)
Injury to the axillary nerve—and resulting paralysis of the deltoid muscle—usually results from shoulder trauma such as dislocation and/or fracture. Motor vehicle accidents, a fall from a height, or a sports injury from skiing, snowboarding, football or rugby are among the common causes. However, axillary nerve palsy may also result from conditions including brachial neuritis and quadrilateral space syndrome.
Birth Palsies
The term birth palsy (or paralysis) refers to injuries to the brachial plexus incurred as the baby emerges from the birth canal. In such instances, the baby’s shoulder is stuck against the mother’s pubic bone during delivery (a condition also referred to as shoulder dystocia), as the head emerges in the other direction, resulting in a traction injury. Infants may have either partial birth palsy, in which only the upper or the lower roots are damaged, or complete birth palsy or avulsion of all the nerve roots. Erb’s palsy is the diagnosis given when the upper roots, usually C5-C6, are affected; Klumpke’s palsy, describes the condition in which the lower roots—C8, T1—are affected. Erb’s palsy is the more commonly seen injury. The inability of the infant to bend his or her elbow is a hallmark of a birth palsy. Nonsurgical treatment may be sufficient if the injury involves a stretched but not disrupted nerve, usually referred to as a neurapraxia. When surgical intervention is necessary, good outcomes can be achieved in appropriately screened patients.
Note: Both Erb’s palsy and Klumpke’s palsy may occur in adults. Erb’s palsy is more likely to result from a motor vehicle injury, such as a motorcycle accident, and Klumpke’s palsy from an injury incurred while hanging on to an object with the body weight suspended from the limb.
Brachial Plexus Injury
The brachial plexus refers to a complex web of large nerves that exit from the spinal cord in the neck and direct the movement and sensation of the entire upper limb. Traumatic brachial plexus injuries, which are most commonly sustained in high-speed motor vehicle accidents or while engaged in sporting events, affect the sensibility and muscle power in part of or the entire limb. Approximately 15% of brachial plexus injuries have an injury to the blood supply of the arm as well, and emergency surgery may be indicated.
Symptoms of Brachial Plexus and Serious Nerve Injury
Patients with injuries to the brachial plexus or other major nerve injuries near the neck or shoulder may have complete or partial loss of function in the arm, with or without sensation. Complete loss of function may also be called flail arm, arm palsy or arm paralysis. Neuropathic or nerve pain is also a sign of serious injury, as is muscle weakness, which is the result of an interruption of electrical signals from nerve to muscle. Treatment of these injuries by many different specialists addresses both the underlying condition and associated pain.
- Complete Plexus: This term refers to brachial plexus injuries in which all five levels of the nerve roots, trunks, divisions, cords and nerves have been injured,( C5, C6, C7, C8 and T1) resulting in total arm paralysis.
- Partial Plexus: Patients with this condition have injury to one or more roots, trunks, divisions, cords or nerves of the brachial plexus, resulting in partial paralysis.
Horner’s Syndrome
This form of brachial plexus injury involves disruption of nerves at the C8 and T1 levels. It is characterized by a drooping eyelid (ptosis), decreased pupil size (myosis), and dryness of the eye (anhidrosis). A drooping eye is often a sign of an avulsion, a complete tear of the nerve from its attachment at the spinal cord.
Double Crush Syndrome
Patients with double crush syndrome have injuries or compression in two separate areas. The most common area is a pinched nerve in the cervical spine as a result of arthritis and disc disease. The other area involves carpal tunnel syndrome, increased pressure on the median nerve of the wrist, or cubital tunnel syndrome, pressure on the ulnar nerve at the elbow. Treatment may be administered in stages, addressing the more significant compression first.
Nerve Compression
A common neck injury in football involves compression or stretching of a nerve root. Referred to as “burners” or “stingers,” they make up approximately 10 percent of all cervical spine neurologic injuries, and two-thirds of all college football players experience at least one of these injuries. These injuries occur from either a pinching (compression) of the nerve on the same side where the neck is flexed/extended or a stretching of the nerve on the opposite side where the neck is flexed/extended.
Those affected may experience sharp, burning pain that may radiate into the shoulder and down the arm to the hand. The symptoms only occur on one side and may include weakness and paresthesia (numbness or tingling) in the involved extremity for several seconds to several minutes. Raising the arm (deltoid), flexing the elbow (bicep), and rotating the arm outwards (using the external rotator muscles of the rotator cuff) may be restricted as a result of motor weakness.
Nerve Injury
Neck injuries are a particular concern in contact sports such as football, and they require special attention because of the devastating consequences if such injuries are severe. Cervical nerve root and spinal cord injuries are among the most common cervical spine neurologic (nerve) injuries.
Nerve Lacerations
Nerve lacerations—cuts or wounds caused by any sharp material, such as glass or metal—accompanied by any difficulty in movement or in sensation, are serious injuries and should be treated immediately. Treatment options vary, depending upon the severity and degree of laceration (partial or complete).
Nerve Pain
Compression or stretching of a nerve root or the brachial plexus can cause a sharp, burning pain that may radiate into the shoulder and down the arm to the hand. The symptoms only occur on one side and may include weakness and paresthesia (numbness or tingling) in the involved extremity for several seconds to several minutes. Raising the arm (deltoid), flexing the elbow (bicep), and rotating the arm outwards (using the external rotator muscles of the rotator cuff) may be restricted as a result of motor weakness.
Nerve Tumors and Nerve Sheath Tumors
Nerves are composed of three layers of protective covering and the nerve fibers or axons inside the nerve that deliver sensory and motor messages between the brain and muscle. Tumors may develop in any portion of the nerve. Removal of a tumor that involves the axons may disrupt nerve function and result in the need for a treatment such as nerve transfer or nerve graft. However, removal of benign nerve tumors of the sheath, such as Schwannomas, will not affect nerve function. Malignant nerve tumors rarely occur.
Neuroma
A condition in which scar tissue has grown around a disrupted nerve.
Neurapraxia
A stretched nerve.
Parsonage-Turner Syndrome (PTS)
Parsonage-Turner Syndrome (PTS), also referred to as idiopathic brachial plexopathy or neuralgic amyotrophy, is a rare disorder consisting of a complex constellation of symptoms with abrupt onset of pain in the shoulder, which is followed by progressive neurologic increasing of motor weakness, a reduced sense of touch, and numbness. Although the cause of the condition is unclear, it has been reported in various clinical situations, including following surgery, following treatment for infections, after an accident or trauma, or after receiving a vaccination. The identification of the syndrome in the postoperative patient remains a challenge as symptoms may easily be attributed to secondary consequence of surgery, recovery, or the anesthetic used for the surgery to block pain. Early recognition and treatment can have improved outcomes for patients.
Thoracic Outlet Syndrome (TOS)
Thoracic outlet syndrome (TOS) is a syndrome that can cause any combination of pain, weakness, numbness, tingling, a cold sensation or, sometimes, a more general type of discomfort in one or both upper limbs. This can be the result of compression of the vascular structures (arteries and/or veins), neurological structures (nerves between the shoulder and neck, known as the brachial plexus), or involvement of both the vascular and neurological structures. Learn more about TOS.
Winged Scapula
As the name suggests, winged scapula is a rare condition in which the shoulder blade juts out in a “wing-like” way from the back causing upper extremity limitations in lifting, pulling, and pushing. The condition results from an injury to the long thoracic nerve, which innervates (supplies nerves stimulus to) the serratus anterior muscle. Once this connection is disrupted, the joint becomes unstable and the scapula “pops” out of place. While usually caused by trauma, including brachial plexus injury, winged scapula may occur as the result of an isolated sports injury or a lymph node biopsy. Some patients with winged scapula are still able to use the arm on the affected side, but prompt treatment is recommended, even in instances when the condition is not caused by traumatic injury. An unstable shoulder may result in other conditions such as bursitis and chronic pain, and difficulty raising the shoulder.
Diagnosis
The brachial plexus refers to a complex web of large nerves that exit from the spinal cord in the neck and direct the movement and sensation of the entire upper limb. Traumatic brachial plexus injuries, which are most commonly sustained in high-speed motor vehicle accidents or while engaged in sporting events, affect the sensibility and muscle power in part of or the entire limb. Although some injuries to the brachial plexus improve on their own, others do not. Approximately 15% of brachial plexus injuries have an injury to the blood supply of the arm as well, and emergency surgery may be needed.
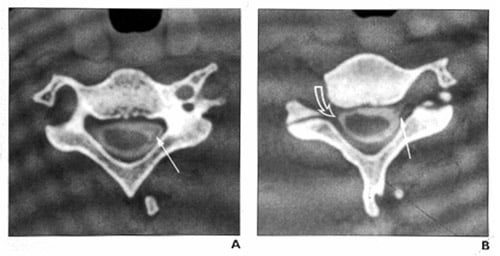
Figures A & B: CT myelogram showing a normal brachial plexus (left) and injured brachial plexus (right)
Exams a Patient Would Undergo
Brachial plexus injuries are unpredictable and usually require additional imaging or electrodiagnostic tests. Frequent and thorough examination over the first three to six months following injury is often necessary to document signs of nerve recovery.
- Physical Exam
An exam would include a physical examination of the upper extremity; starting with a neurologic examination, which is critical in evaluating upper extremity conditions, including neck, vascular, motor, sensory, and reflexes. The examiner would try to recreate symptoms sometimes associated with such an injury by having the patient bend his or her neck back and forth in various positions.
- Neurologic Exam
- Elbow Exam
- Hand and Wrist Exam
- In additional to performing a physical examination, orthopedists often evaluate brachial plexus injuries using MRIs, CT scans, and electrodiagnostic tests.
- Electromyography (EMG) Testing
Electromyography (EMG) is a form of electrodiagnostic testing that is used to study nerve and muscle function and can provide specific information about the extent of nerve and/or muscle injury, the location of the injury, and give some indication whether the damage is reversible.
For more information about EMG testing, see A Patient’s Guide to EMG Testing
Rehabilitation
An award-winning staff of occupational and physical therapists with specialized training and clinical expertise.
When patients experience traumatic injury to the nerves in the brachial plexus or other peripheral nerves that serve the hand, arm or shoulder, they often lose function and sensation in some or all of the affected limb. Whether or not surgery is required, commitment to a long-term physical therapy program is a key step toward recovery and can make the crucial difference in long-term ability to function.
As members of the multidisciplinary team that provides care at the Center for Brachial Plexus and Traumatic Nerve Injury at Hospital for Special Surgery (HSS), it is beneficial if physical and occupational therapists get involved as soon as the patient is diagnosed, explains Alexandra MacKenzie, OTR/L, CHT, with the Hand Therapy Center at HSS. "At that point our role is to assess the patient's strength and range of motion. We begin a regimen of exercises adapted to the specific injury as soon as the patient has medical clearance."
Rehabilitation While Monitoring an Injury
For some patients, those with neurapraxia (a nerve that has been stretched, but not disrupted or severed) for example, the course of treatment involves several months of monitoring by the Center for Brachial Plexus and Traumatic Nerve Injury team to see if the nerve will recover on its own. During this period, physical therapy helps the patient to maintain the injured limb's range of motion and prevents unaffected muscles from atrophying. Movement is also important to help treat edema or swelling in the area, which can contribute to stiffness.
Sometimes a patient will wear a splint as part of his or her post-injury recovery. For example, if the patient is unable to use the muscles that control the wrist, the joint flexes forward in an abnormal position. Splinting helps hold the wrist in a neutral position during recovery—thereby protecting it and preventing possible contractures from developing that may limit movement.
Rehabilitation Following Surgery
Those who undergo a surgical procedure, such as a nerve graft or a nerve transfer to repair their injury, may start gentle exercises the first day after their surgery. "In the beginning, the exercises may be passive," explains Ms. MacKenzie. "If the patient can't move the limb, the therapist or, eventually, a trained family member or caregiver, does it for them."
Retraining the Brain and Restoring Nerve Connections to the Limb
Retraining the brain to send information along grafted nerve tissue or along a new nerve pathway is the long-term and ultimate physical therapy goal for these patients. For example, a patient who has undergone a procedure in which the nerve that once served the muscles surrounding the ribcage has been rerouted to deliver electrical information to the bicep must be retrained to contract the bicep. In this case, deep breathing may be the initial exercise used to help activate the new connection.
Another technique involves the use of mirrors. The patient's injured arm is placed behind a mirror while he or she watches the reflection of the unaffected arm in the mirror move. This is a way of "tricking" the brain into thinking the injured arm is moving, and helping to restore connection to that limb. "It's very exciting to see the connection and therefore movement come back," Ms. MacKenzie adds. Crunches, abdominal exercises and cardiac activity can all play a role in recovery as well.
A Long-term Recovery Process
Because nerve regenerates very slowly, patients may not see results for six months or even a year after surgery. Progress often continues several years following surgery. "We help patients understand that it's important to keep moving to maintain joint flexibility, even if they're not seeing immediate results. Otherwise, even if the nerve is eventually able to reactivate the muscle, if the joint is stiff, function will still be impaired," says Ms. MacKenzie.
Biofeedback
Biofeedback is sometimes used to help patients stay motivated and assess their progress. To use the mechanism, an electrode is attached to the skin over the affected muscle. As the muscle contracts, the electrode transmits information to the machine that registers the strength of the contraction. This information is then communicated back to the patient through lights on a bar and with a sound emitted by the machine. As the muscle contractions grow stronger, the lighted bar becomes longer and the beeping sound becomes louder. "This is a great exercise to use early on in the patient's therapy. Even if they can't gauge how much they're contracting the muscle, and even if they're not seeing movement in the muscle, the machine lets them know that it's happening. It's just one more tool we can use to help create that pathway between brain and muscle," says Ms. MacKenzie
Helping Recovering Patients Perform Day-to-Day Activities
During recovery, therapists also assist with adaptive techniques for one-handed dressing, bathing and other daily activities. If the patient is unable to use the hand he or she writes with, therapeutic techniques can also train the other hand to perform this function.
A Resource for Therapists Close to Home
Because patients come from all over the country to seek care at the Center for Brachial Plexus and Traumatic Nerve Injury, the therapists at the Center have experience in helping patients find programs close to home, once their initial treatment is completed.
Helping Patients Establish Goals
"We spend a lot of time with patients helping them establish realistic goals and expectations and encouraging them to remain motivated. Because we see them over and over again, we have the opportunity to keep discussing their progress," says Ms. MacKenzie. "In the beginning these injuries can be so overwhelming; it can be hard to absorb all the information about recovery at once."
Additional Rehabilitation Resources
Brachial Plexus and Traumatic Nerve Injury Frequently Asked Questions
-
Is there a way to fix my arm?
A traumatic injury to the brachial plexus (nerves that conduct signals to the shoulder, arm and hand) can have devastating consequences, including loss of function and chronic pain, for an otherwise healthy, active patient. Fortunately, new advances in nerve surgery can yield marked improvement in movement and function in the shoulder, elbow and hand while simultaneously diminishing pain.
-
Can a brachial plexus injury be treated?
Early recognition and treatment of this injury, along with the recent advances that have been made in microsurgical reconstruction, have greatly improved outcomes for patients. Injuries for which restoring function would have been impossible only two decades ago are now being treated with nerve reconstruction, increasing the possibility of a return to an active productive life. The Center for Brachial Plexus and Traumatic Nerve Injury at Hospital for Special Surgery in New York City leads a multidisciplinary approach to expertly treat injuries of the brachial plexus and peripheral nerves.
-
Can my movement be restored?
New advances in nerve surgery can yield marked improvement in movement and function in the shoulder, elbow and hand while simultaneously diminishing pain.
-
How long should I wait before being evaluated for my nerve injury?
Injuries to the brachial plexus should be evaluated as soon as possible. A physician can help the patient decide on the need for more diagnostic procedures and discuss the likelihood of spontaneous recovery, and the timing of surgery, if indicated. Ideally, if surgery is required, it should be completed within six months of the date of injury.
-
I think I may be a candidate for nerve transfer surgery. Do I need a referral from my regular physician?
If you have been diagnosed with a traumatic brachial plexus injury, you may call our office directly. If you are not certain whether you may have injured your brachial plexus, you should check with your primary care provider or a neurologist.
-
How will I be evaluated at HSS?
A team of physicians, nurses, research personnel, and specialized hand therapists evaluates each patient and continues to work with him or her throughout the course of treatment. Specialized testing may be required, including computerized tomography (CT), myelography, magnetic resonance imaging (MRI), and neurodiagnostic testing. A physician at the Center will fully evaluate each patient before advanced imaging or neurodiagnostic tests are ordered, so that a customized approach can be mapped, and unnecessary or duplicate testing avoided.
-
How long does this procedure take and when will I be able to return to my regular activities?
Surgery for a brachial plexus injury can range from 3 to 12 hours, depending on the complexity of the case. Patients can expect to restrict their activities for at least four weeks following surgery; therapy for the upper extremity may be necessary for several months while nerves and muscles recover.
-
How long will I be in the hospital?
Most patients are discharged the day following surgery. However, in some cases, the procedure may be done on an outpatient basis.
-
Where will the orthopedic surgeon get the nerve that will be transferred?
The nerve that is transplanted is usually taken from an uninjured muscle in the same area as the non-working muscle. It’s important to understand that the entire nerve is not transferred; only a portion is moved, so that function and sensation are not affected in uninjured areas. On occasion, a nerve graft from the leg is used if more nerve tissue is required. (Scott W. Wolfe, MD has presented his success using bioabsorbable nerve conduits; tiny chambers that span gaps between damaged nerves, and allow nerves to grow and repair injured nerves.)
-
What do the surgical scars look like?
The appearance of scars may vary. The incisions can be a few inches in length and occasionally quite extensive, depending on the degree of injury. Plastic surgical techniques are used to close the incisions to minimize scarring. Some examples of postsurgical scars are below.

Examples of postsurgical scarring after brachial plexus repair
-
Is there much postsurgical pain?
Surprisingly little pain is associated with surgery for brachial plexus injuries. If needed, pain management specialists at HSS have extensive experience in helping patients feel comfortable throughout their recovery.
-
How can I cope with the crushing/burning pain in my arm? Will surgery make it go away?
For most patients, relief from the pain associated with brachial plexus injury (as distinguished from postsurgical pain) is achieved at one or two years following surgery, although in some cases a longer period of time may elapse before the pain is controlled. For those individuals who continue to experience pain beyond this period, the orthopedic surgeon may make a referral to a neurosurgeon, who may recommend an additional surgery on the spinal cord known as Dorsal Route Entry Zone lesioning (DREZ). DREZ involves the removal of scar tissue and the use of an electrode on the damaged area of the spinal cord to stop pain messages from being sent to the brain.
-
If my surgery is successful, is there any chance the problem will recur?
No, as long as a patient does not experience another injury to the area.
-
What kind of physical therapy will I do?
Physical therapy for the upper extremity is essential. The program usually begins before any surgical intervention and continues for many months following surgery. Pool therapy is particularly important and biofeedback may also be helpful.
-
What kind of risks are associated with this type of surgery?
Risks associated with surgery to repair a brachial plexus injury include failure to improve, tingling or diminished strength in areas of the hand or forearm (generally temporary), and post-surgical stiffness. The surgery can be long, and the resulting pressure to certain areas of the body can cause temporary pain; great efforts are made to pad these areas with special gelpads during surgery.
-
Why wasn’t my brachial plexus injury treated at the time of my accident?
When the injury is incomplete, it is prudent to wait to see if a brachial plexus injury will improve spontaneously. In many cases, this recovery does occur and surgery is not needed. Often the nerve injury cannot be fully appreciated immediately, and may be overshadowed by life-threatening injuries of the skull and brain, abdomen, or fractures and dislocations of the shoulder and arm. In more serious cases, repair of critical blood vessels to the arm may be necessary for the limb to survive, and nerve repair is planned as a subsequent, elective procedure.
“One of the goals for the Center for Brachial Plexus and Traumatic Nerve Injury at Hospital for Special Surgery is to be a resource to hand and upper extremity medical professionals around the world.”
The Center for Brachial Plexus and Traumatic Nerve Injury is a nationally recognized health resource for men and women of all ages providing diagnostic and reconstructive options for patients with injuries or dysfunction of the peripheral nerve and brachial plexus.
Using a multidisciplinary approach, the Center utilizes the expertise of a wide range of health care professionals including orthopedic surgeons, physiatrists, neurologists, radiologists, psychiatrists, rheumatologists, pain management specialists, physical therapists, and anesthesiologists so that patients can benefit from a coordinated treatment experience.
In addition to improved patient treatment and outcomes, central to the mission of the Center is creating continuing education programs for the broader medical community. Primary care physicians, specialty physicians (including orthopedics, anesthesiology, neurology and physiatry), physical therapists, athletic trainers, physician assistants, nurse practitioners, residents, fellows and medical students will benefit from an increased understanding of brachial plexus anatomy, injury patterns and potential treatments.
How to Refer Your Patient
You or your patient can call the Center by telephone weekdays between 9am and 5pm ET. On evenings and weekends, leave a voice message and we will return your call.
HSS eAcademy® Surgical Videos and CME Programs
The HSS Education Institute offers a range of on-site professional and continuing medical education programs related to dysfunction of the peripheral nerve and brachial plexus.
- View professional education surgery videos focused on the brachial plexus, as well as on other hand and upper extremity conditions.
- Browse all available HSS eAcademy CME programs.
Related Services
Combining the medical expertise of specialists and researchers in the fields of orthopedics, physiatry, neurology, rehabilitation, radiology and imaging, and prosthetics and orthotics, the Center is leading the way in diagnosis and treatment of brachial plexus and complex nerve injuries with the best and most advanced medical care.
Neurology
Neurologists at HSS perform general neurological consults for adults and neuromuscular consultations for adults and pediatric patients with various nerve and muscle diseases. All medical staff members of the department are board-certified neurologists with subspecialties in neurophysiology and neuromuscular diseases.
Physiatry
Physiatrists at HSS perform non-operative treatment procedures on patients who have spinal and sports-related injuries as well as other musculoskeletal problems. Several members of the department also perform electrodiagnostic studies such as nerve conduction and electromyography. These diagnostic studies help to determine whether patients may have nerve or muscular disorders.
Pain Management
Whether pain stems from nagging back pain, an acute sports injury, a recent operation, osteoarthritis or complex regional pain syndrome, our specialty-trained pain management physicians are driven to understand and eliminate it. In our patient-centric care model, patients are evaluated and treated by physicians with the interest, clinical expertise, cutting-edge training and skill to relieve pain and restore life.
Rehabilitation
HSS Rehabilitation plays an integral role in patient care and research at the Hospital. Its skilled professionals provide quality rehabilitative care for patients of all ages pre-operatively, post-operatively, and/or for conservative management of musculoskeletal injuries and conditions.
Hand Therapy Center
The Hand Therapy Center provides upper extremity rehabilitation services designed to insure optimal restoration of function. Its award-winning staff includes occupational and physical therapists with specialized training and clinical expertise in hand therapy.
Radiology and Imaging
The Department of Radiology & Imaging at HSS is nationally and internationally recognized as the premier center for leading edge musculoskeletal, orthopedic, and rheumatologic clinical and research imaging. Approximately 250,000 musculoskeletal imaging examinations are performed annually including Magnetic Resonance Imaging (MRI), Computed Tomography (CT), and Ultrasound, of which approximately 180,000 are conventional radiography (X-ray) and interventional procedures.
Prosthetics and Orthotics
The Prosthetics and Orthotics Service at HSS includes a comprehensive, world-class facility capable of fitting, crafting, modifying, fabricating, and delivering prefabricated and custom prosthetic limbs and orthotic appliances which are tailor-made for any orthopedic condition.
See a physician at the Center for Brachial Plexus and Traumatic Nerve Injury:
Video: What is Nerve Transfer Surgery?
What is nerve transfer surgery? What is a brachial plexus injury? Watch our experts speak on these topics and learn more about the HSS approach to diagnosing and treating these musculoskeletal injuries and conditions.
In the News
- Liposomal Bupivacaine Shows Similar Length of Pain Relief as Standard Bupivacaine With Dexamethasone After Shoulder Surgery
- 10 orthopedic surgeons to know
- Innovative Surgery Restores Muscle Strength and Movement In Patients Experiencing Paralysis from Parsonage-Turner Syndrome
- HSS Researchers Launch Study Using Novel MRI Techniques to Find a Biomarker for Parsonage-Turner Syndrome, A Painful Nerve Disorder
- HSS Names Steve Lee, MD, new Chief of Hand, and Ernest Sink, MD, new Chief of Hip Preservation
- Surgeon from Greenwich finds solution to puzzling paralysis in children
- Superior Trunk Block: A Safer Shoulder Surgery Anesthesia Alternative to the Interscalene Block for Patients With Compromised Pulmonary Function
- Pioneering Surgery Restores Movement to Children Paralyzed by Acute Flaccid Myelitis
- HSS presents new research at 2018 AAHS Annual Meeting
- HSS researchers develop brachial plexus surgery, surgical outcomes impact assessment: 4 key insights
- What is the Most Optimal Nerve Transfer for Brachial Plexus Patients?













