Treating Tibial Nonunion and Multilevel Deformity with Distraction Osteogenesis and Ring Fixator with 6-Axis Correction in a 10-Year-Old Girl
From Grand Rounds from HSS: Management of Complex Cases | Volume 11, Issue 1
Case Report
A 10-year-old girl presented after she was diagnosed with right proximal tibial osteomyelitis 5 years prior. She underwent surgical irrigation and debridement followed by a 6-month course of intravenous antibiotics. Approximately 1 year postoperatively, she developed a progressive, painful varus deformity of her right tibia and a significant leg length discrepancy.
On examination, she ambulated with a varus thrust of the right lower extremity and a significant limp. A 4-cm block under her right foot produced a functionally level pelvis. She reported pain in the right proximal tibia with ambulation. A large, non-tender bony prominence over the lateral aspect of the proximal tibia at the apex of her varus deformity was noted. She demonstrated no range of motion limitations or neurovascular deficits.
Initial radiographs demonstrated a 34° varus deformity of the right proximal tibia secondary to a hypertrophic nonunion (Fig. 1A–C), as well as a proximal tibial recurvatum deformity secondary to premature asymmetric closure of the proximal tibial growth plate. Full length standing radiographs demonstrated a roughly 4-cm leg length discrepancy. Computed tomography (CT) and magnetic resonance (MR) imaging of the right tibia confirmed fibrous nonunion of the proximal tibia, without radiographic evidence of ongoing infection. Laboratory values were within normal limits.
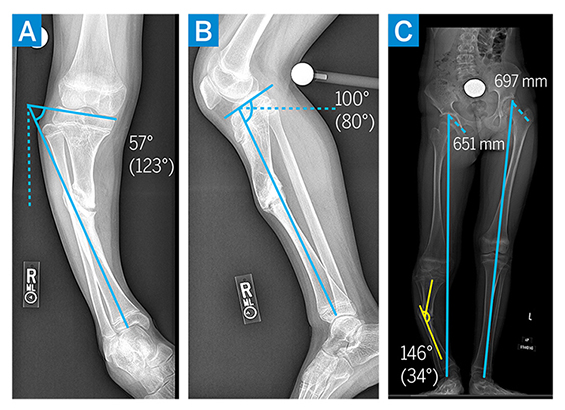
Figure 1: (a–c) Preoperative imaging demonstrating varus and recurvatum deformity of the right proximal tibia diaphysis with associated limb leg length discrepancy.
The patient underwent right proximal tibial epiphysiodesis, fibular osteotomy, and distraction osteoplasty with a hexapod frame. The nonunion was found to be nonosseous and hypertrophic in nature, allowing for correction through the nonunion site without need for additional osteotomy. The intramedullary canal proximal and distal to the nonunion site was drilled, and intraoperative cultures were obtained to confirm absence of ongoing infection. A hexapod ringed external fixator was applied to allow for simultaneous correction of the varus deformity and gradual lengthening (Fig. 2A). By 2 months postoperatively, the patient’s varus deformity was significantly improved and limb length discrepancy had improved to 3 cm (Fig. 2B–C). Her external fixator was removed 3 months postoperatively, with a residual recurvatum deformity noted (Fig. 3A–B). Shortly thereafter, she underwent right proximal tibial metaphyseal osteotomy and gradual deformity correction with a hexapod ringed external fixator (Fig. 3C). By 3 months postoperatively, coronal and sagittal alignment were normalized and the external fixator was removed (Fig. 3D).
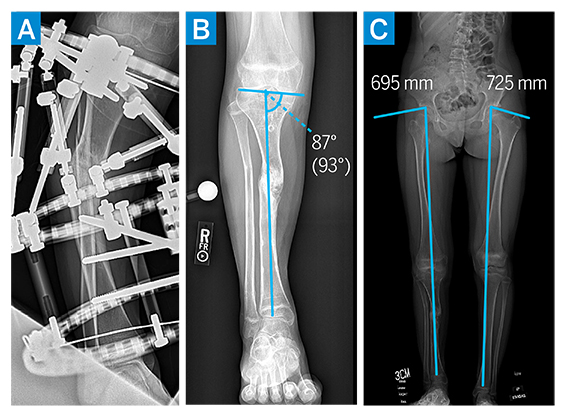
Figure 2: (a–b) Perioperative imaging demonstrating tibial intramedullary canal drilling and frame placement. (c) At 3 months postoperatively, imaging demonstrated improved alignment and leg length discrepancy.
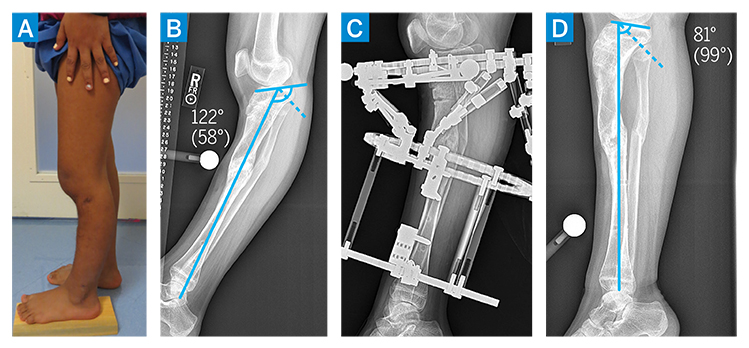
Figure 3: (a–b) Preoperative imaging demonstrating persistent recurvatum deformity. (c–d) Postoperative imaging demonstrating external fixator and proximal tibia osteotomy, resulting in normalization of tibial slope.
Currently, 1.5 years from the primary nonunion correction and 6 months from the proximal tibia recurvatum deformity correction, she participates in all activities without pain or limitations. At the most recent examination, radiographs demonstrated maintenance of surgical correction of tibial slope and mechanical alignment, with healed nonunion and osteotomy and improved leg length discrepancy (Fig. 4A–E). She will be monitored annually until skeletal maturity for leg length discrepancy and lower limb alignment.
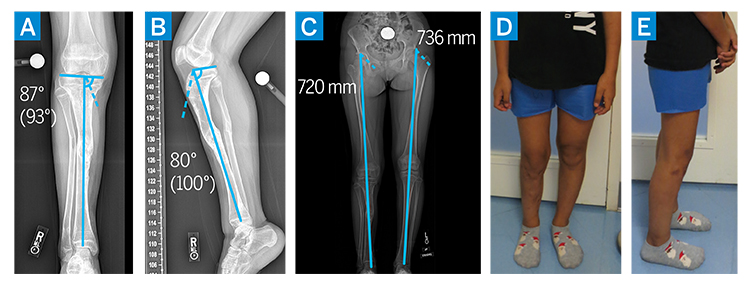 Figure 4: (a–e) Postoperative imaging demonstrating correction of varus and recurvatum deformities, with normalization of mechanical alignment and improvement in leg length discrepancy.
Figure 4: (a–e) Postoperative imaging demonstrating correction of varus and recurvatum deformities, with normalization of mechanical alignment and improvement in leg length discrepancy.
Discussion
Osteomyelitis is relatively common in children, with the tibia the most affected long bone [1]. Initial treatment focuses on eradicating the infection through intravenous antibiotics and surgical debridement. Still, long-term sequelae may result from osteomyelitis, including angular deformities, fractures, physeal arrest, and deep vein thromboses [1]. Tibial nonunion is particularly difficult to treat and may be associated with significant functional limitations. In children, the presence of open physes must be considered; maintaining continued longitudinal growth and restoring coronal and sagittal limb alignment are essential during deformity correction.
Operative treatments of long bone nonunion may include plate osteosynthesis, intramedullary nailing, autograft or allograft augmentation, and bone stimulators. Distraction osteosynthesis through the nonunion site, a technique developed by Ilizarov for both adults and children, may be especially useful in cases of multiplanar correction, with low rates of recurrence [2-4].
In this case, a deformity resulting from infection created a diaphyseal nonunion, varus alignment, and proximal tibia metaphyseal recurvatum deformity. Because there were 2 deformities at separate levels, resolving the deformity through a single site would have produced significant residual deformity at 1 of the levels. The Ilizarov method of distraction osteogenesis allows for resolution of the stiff hypertrophic nonunion, correction of the varus deformity, and slight lengthening at the diaphyseal nonunion site. The patient may maintain full weight-bearing and joint range of motion above and below the nonunion site while in the frame. The 6-axis system permits correction of all axes of deformity simultaneously [4,5]. The minimally invasive approach and the versatility of the planning software and frame allow for real-time feedback and adjustment of weight-bearing alignment.
Posted: 2/18/2022
Authors
Tyler Uppstrom, MD
Orthopaedic Surgery Resident
Arkady Blyakher, MD
Specialist Assistant
Pediatric Orthopaedic Surgery
Limb Lengthening and Reconstruction
Attending Orthopedic Surgeon, Hospital for Special Surgery
Professor of Clinical Orthopedic Surgery, Weill Cornell Medical College
References
- Stone B, Street M, Leigh W, Crawford H. Pediatric Tibial Osteomyelitis. J Pediatr Orthop. 2016 Jul-Aug 2016;36(5):534-40. doi:10.1097/ BPO.0000000000000472
- Ashfaq K, Fragomen AT, Nguyen JT, Rozbruch SR. Correction of proximal tibia varus with external fixation. J Knee Surg. Nov 2012;25(5):375-84. doi:10.1055/s-0031-1299659
- Saw A, Phang ZH, Alrasheed MK, Gunalan R, Albaker MZ, Shanmugam R. Gradual correction of proximal tibia deformity for Blount disease in adolescent and young adults. J Orthop Surg (Hong Kong). 2019 Sep-Dec 2019;27(3):2309499019873987. doi:10.1177/2309499019873987
- Koren L, Keren Y, Eidelman M. Multiplanar deformities correction using taylor spatial frame in skeletally immature patients. Open Orthop J. 2016;10:71-9. doi:10.2174/1874325001610010603
- Abuomira IE, Sala F, Elbatrawy Y, Lovisetti G, Alati S, Capitani D. Distraction osteogenesis for tibial nonunion with bone loss using combined Ilizarov and Taylor spatial frames versus a conventional circular frame. Strategies Trauma Limb Reconstr. Nov 2016;11(3):153-159. doi:10.1007/s11751-016-0264-4
