Youth Sports Injuries and Conditions
Summary: As more children and teens playing competitive athletics, youth sports and exercise-related injuries and conditions are on the rise. When not properly treated, injuries in a child can have long-lasting effects that, especially with concussions, can cause more problems than in adults. This article explains how the anatomy of growing children and adolescents affects diagnosis and treatment of fractures, injuries, and multiple conditions.

Some injuries in children mirror those seen in adult athletes: fractures, sprains, and torn ligaments, for example. But injury patterns, required techniques for proper diagnosis, and choices of treatment can vary significantly in growing kids. It is recommended that an injured child see a physician who specializes in pediatric medicine to address all of the concerns related to recovering from a youth sports injury or condition.
Most youth injuries or athletic conditions require:
- Time-off to heal from the injury
- Rehabilitation and physical therapy
- Performing preventative exercises
- Maintaining proper form and technique in activity
Ask the Expert: Dr. Tiana S. Woolridge on youth sports injuries
Growing bodies are different from those in adults. Children and teens who participate in athletics and experience an acute or overuse injury should be seen by a sports medicine specialist with pediatric medical expertise.

Youth Sports and Injuries: What Every Parent and Coach Should Know
Common sports injuries in children and teenagers
Some of the most frequently seen injuries in youth sports are:
ACL tears in children and adolescents
Partial or complete tears of the anterior cruciate ligament (ACL) – which is part of a complex of ligaments that help stabilize and support the knee joint – are often associated with sports that involve pivoting. Some examples include soccer, lacrosse, football, basketball, field hockey, and skiing.
As in adults, ACL injuries are more common among female athletes than in males, perhaps owing to anatomic differences in the knee, as well as mechanical differences in the way that males and females move, jump, and land.
When an adult ruptures an ACL, it’s usually the ligament that is disrupted. In children, because the ligament may be stronger than the bone, the ligament may, instead of tearing in mid-substance, pull away from its attachment to the tibia with a small piece of bone attached. This type of injury (also known as tibial spine fracture or a tibial eminence fracture) can be surgically repaired, often with the use of arthroscopic or minimally invasive techniques. Following recovery, the child’s ACL is usually restored to normal function.
By strengthening the thigh muscles, the quadriceps, and hamstring muscles, some ACL injuries can be avoided. HSS has developed an ACL injury prevention tip sheet with exercises and drills to help young athletes develop strength and minimize injury.
Growth plate injuries
The ends of some long bones in children, where growth continues until they reach skeletal maturity (known as epiphysial or growth plates) contain less calcium than those of adults. Therefore, injuries at a growth plate can look different on routine X-rays, making some fractures difficult to correctly diagnosis.
Unlike with fractures in adults, MRI and/or ultrasound imaging is needed to obtain more information about the injury.
HSS scientists and clinicians developed a new technique for obtaining images of growth plate injuries in children can now help guide treatment decisions. The technique provides computer-generated 3D models obtained from MRIs that surgeons can use in the operating suite to achieve optimal results.

3D models of growth plate injuries obtained from MRIs offer greater precision and speed with less radiation than CT imaging.
In healthy children, new bone tissue develops from the growth plate, or physis, which is located at either end of the long bones. Physeal bars – bony tissue that forms across the growth plate after trauma – can result in either a deformity or a shortened limb. If the bar covers less than 50 percent of the growth plate, surgical removal can restore normal bone growth.
When treating children, a pediatric orthopedist must take into account potential damage to the growth plate. Tri-plane fractures (a complex type of ankle fracture) constitute one such injury. Seen only in adolescents and sometimes mistaken for sprained ankles, these fractures require prompt attention and often surgery. Growth plate fractures of the knee can also be difficult to diagnose. Some growth plate fractures may be treated conservatively, while others can require surgical correction. Improperly treated, these injuries may result in deformity and altered growth of the affected joint.
Osteochondritis dissecans
Osteochondritis dissecans (OCD) is a condition that develops in the knee, specifically in the cartilage and underlying bone that lines the end of the femur (the long bone in the upper leg) where it meets the tibia in the lower leg to form the knee joint.
Thought to be the result of repeated micro-trauma (small stress injuries), the condition causes pain and disability. In severe cases, a small piece of bone may break loose into the knee joint. Fortunately, in 90% or more of OCD cases, the patient can make a complete recovery with rest and activity modification for a period of three to six months.
For more severe cases, HSS surgeons surgically reposition the bone fragment and secure it in place using a biodegradable screw or nail. One such device, the SmartNail®, was developed by HSS surgeon Russell F. Warren, MD. Together with rest and physical therapy we have a very high success rate in treating these patients.
Discoid meniscus
The term “discoid meniscus” describes a congenital condition in which the meniscus, a cartilage pad found in the knee joint, is formed in a disc shape rather than the normal C-shape found in most individuals.
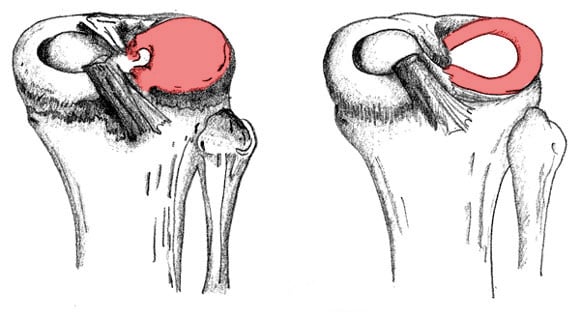
Diagram of a discoid meniscus (L) and a normal meniscus (R).
Note the backwards C-shape of the meniscus on the right. Illustration by Mac O'Conor.
Some people with discoid meniscus never experience any symptoms and do not require treatment. However, if a child with discoid meniscus is experiencing pain and mechanical symptoms, such as stiffness or locking, surgery may be recommended.
Using arthroscopic techniques, the orthopedic surgeon sculpts the meniscus into the more anatomic C-shape. If the areas where the cartilage attaches to the bone are found to be loose (a condition that is sometimes found with discoid meniscus), they can be reaffixed during the same procedure.


