Chronic Periprosthetic Joint Infection in an Immunocompromised Patient Treated With 2-Stage Revision and a Spacer Exchange
From Grand Rounds from HSS: Management of Complex Cases | Volume 13, Issue 1
Case Report
A 51-year-old man presented with an infected right total hip arthroplasty (THA). He had undergone a posterior THA at another institution in 2018 without perioperative complications. He had a history of chronic renal failure requiring dialysis and was awaiting a donor kidney. Hip discomfort began 6 months postoperatively, when his surgeon diagnosed loosening. When he presented to HSS he was diagnosed with septic loosening, with a hip aspiration positive for Klebsiella. Surgical intervention was postponed because of kidney transplantation, which was not successful, and the patient required further dialysis. The hip components continued to show evidence of septic migration, causing extreme pain.
On examination, a 1.5-cm leg length discrepancy and limited hip flexion of 0 to 45° were noted. Radiographs showed septic loosening of the femoral and acetabular components with lytic areas around the acetabular component and around the proximal femur with bony remodeling (Fig. 1). Repeat aspiration was positive for Pseudomonas and methicillin-sensitive Staphylococcus aureus.

Figure 1: Preoperative radiograph shows THA with marked cystic osteolysis around the femoral component with subsidence, concerning for septic loosening. No fracture is identified. There is subluxation of the femoral head from within the acetabular component.
After a period of medical optimization, the patient underwent explantation, irrigation and debridement, and insertion of an articulating spacer. Despite proximal femoral bone loss, we preserved the proximal femur due to the patient’s young age and placed a 200-mm collared femoral component (Stryker Eon) coated proximally with antibiotic cement. We placed a semi-constrained polyethylene acetabular spacer component and used high-viscosity cement (Palacos R+G) containing gentamicin 0.5 g, vancomycin 2 g, and tobramycin 1.2 g per bag, with methylene blue incorporated (Fig. 2). Postoperatively, the patient was 20% weight-bearing on the leg with the foot flat and received a 6-week course of IV minocycline and levofloxacin. After a 2-week antibiotic holiday, repeat aspiration revealed concern for persistent periprosthetic joint infection (PJI), with a synovial white blood cell count of 4867 cells/μL with an 89% differential for neutrophils. The team had concerns that osteomyelitis was present in the proximal femur and that resection would be required.
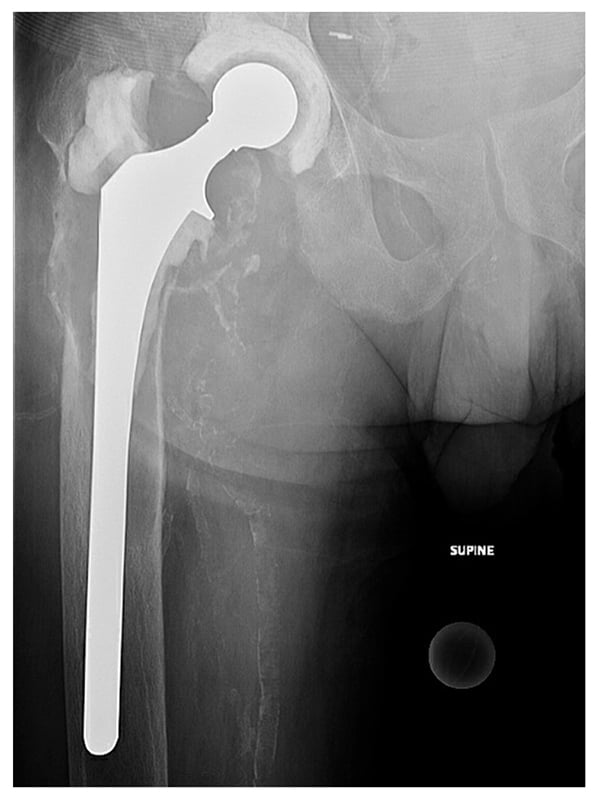
Figure 2: Postoperative radiograph shows an articulating hip spacer with a semi-constrained acetabular component and long femoral component coated proximally with antibiotic cement.
The patient underwent spacer removal, proximal femur resection, and proximal femoral spacer insertion. A Dall-Miles cable was placed around the proximal femur due to severe osteoporosis in this bony segment (Fig. 3). The patient once again was placed on limited weight bearing and IV antibiotics. After a 3-month antibiotic holiday, blood work and aspiration showed no infection. The patient then underwent reimplantation with a 68-mm multi-hole revision acetabular component. The ectatic, stovepipe femur precluded use of a modular tapered stem due to fracture concerns, and the history of recurrent infections precluded use of impaction grafting with cadaveric bone due to recurrent infection concerns.
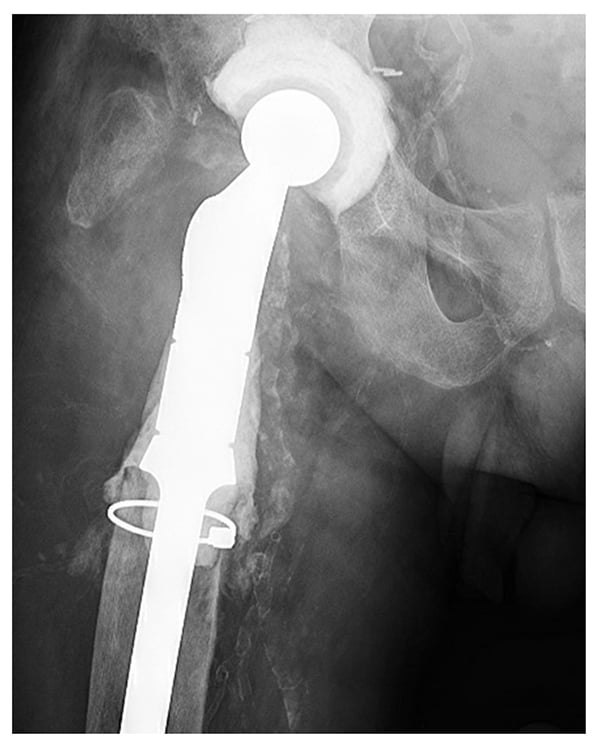
Figure 3: Postoperative radiograph shows the revised articulating hip spacer with a proximal femoral replacement with a proximally coated stem with antibiotic cement. The acetabular component has been changed.
A trial with a proximal femoral replacement (Stryker GMRS) revealed that the largest size, 18 mm, was still significantly smaller than the diameter of the diaphysis. Therefore, we used a construct more common in distal femoral replacement, the Stryker tibial cone system, with gentle hand preparation of the diaphyseal orifice. With the cone trial in place, the proximal femoral trial had better axial and rotational stability. We placed a size-C Stryker cone that was impacted in place, as well as a proximal femoral stem (size 15 × 127 mm) fixed with vacuum mixed cement containing gentamicin and vancomycin (Fig. 4). A dual mobility liner was placed to minimize the risk of instability. The intraoperative cultures were negative and postoperatively the patient had a similar restriction and weight bearing of only 20% for 3 months. He then began weight bearing with a cane, with minimal pain and no apparent leg length discrepancy.

Figure 4: Most recent radiograph shows a highly porous revision acetabular component and cemented proximal femoral replacement with a diaphyseal engaging tibial cone.
Discussion
The treatment of PJI in an immunocompromised patient is challenging. Dialysis and organ transplant patients face significantly higher risks of perioperative complications and treatment failures. In this case, the initial attempt at preserving bone likely caused the first explant procedure to fail, revealing the importance of distinguishing PJI and simultaneous osteomyelitis. Extensive osteoporosis secondary to chronic renal disease and bone loss secondary to femoral component loosening produced a challenge for diaphyseal-based reconstruction.
While a metaphyseal or diaphyseal cone and a cemented diaphyseal stem can be employed in revision knee surgery when the distal femur is compromised, this case is just the third to be reported of their use in the proximal femur [3,4]. The eccentric position of the diaphyseal portion of the stem illustrates the difficulty in assessing construct alignment when faced with a stovepipe femur. Longer-term follow-up and a case series are needed before this approach can be recommended for routine use in such challenging situations.
References
- Khanna V, Sakthivelnathan V, Senthil T, et al. Dialysis patients undergoing total hip arthroplasty have higher rates of morbidity and mortality and incur greater healthcare costs: a national database study from 367,894 patients. Indian J Orthop. 2022;57(2):336-343.
- Chou TA, Ma HH, Tsai SW, et al. Dialysis patients have comparable results to patients who have received kidney transplant after total joint arthroplasty: a systematic review and meta-analysis. EFORT Open Rev. 2021;6(8):618-628.
- Koech H, Lawrenz JM, Mesko DR, Molloy RM. A novel use of a tibial cone in a proximal femoral replacement. Arthroplast Today. 2018;4(2):175-179.
- Ramos MS, Rullan-Oliver P, Pasqualini I, Piuzzi NS, Molloy RM. Revision total hip arthroplasty using a tibial cone and impaction grafting for severe femoral bone loss: a case report. JBJS Case Connect. 2023;13(3).

