Treating Massive Glenoid Bone Deficiency with a Custom Metal Glenoid Implant
From Grand Rounds from HSS: Management of Complex Cases | Volume 10, Issue 1
Case Report
A 63-year-old man presented for evaluation after several years of increasing right shoulder pain. While serving in the Vietnam War, he had sustained a shrapnel injury to his right shoulder and developed proximal humerus osteomyelitis, requiring multiple irrigation and debridement procedures. He subsequently developed severe glenohumeral arthritis and underwent several years of conservative management including nonsteroidal anti-inflammatory drugs and steroid injections.
Radiographs showed severe glenohumeral arthritis (Fig. 1). His range of motion was forward elevation 70°, external rotation −10°, internal rotation to the side with pain throughout the motion arc. Infections workup showed erythrocyte sedimentation rate of 10 mm/hr, C-reactive protein level of 1.12 mg/L, and white blood cell count of 5.3 × 109/L. He elected to proceed with shoulder arthroplasty as a staged procedure. A custom molded antibiotic spacer was placed as a hemiarthroplasty, and the patient completed a 6-week course of antibiotics. Intraoperative cultures showed no growth, and a reverse shoulder arthroplasty was planned as the second stage of the procedure.

Firgure 1: X-rays of the right shoulder show severe glenohumeral arthritis.
Computed tomography with 3D reconstruction was used preoperatively and showed bony deficiency with a compromised glenoid vault (Fig. 2). The Comprehensive® Vault Reconstruction System (VRS) (Zimmer Biomet, Warsaw, IN) was planned with computer-aided design (CAD) software to create a custom titanium implant. The software allowed for planning of exact screw trajectories to obtain the best purchase in the remaining scapular bone.
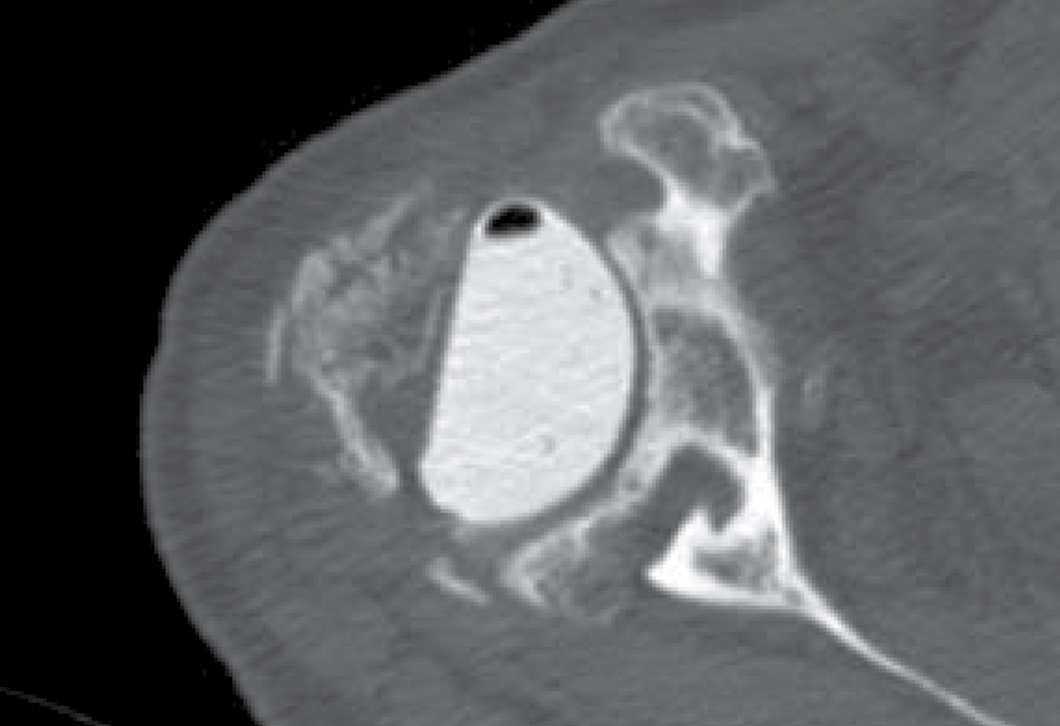
Figure 2: CT with 3D reconstruction shows deficient glenoid vault.
The previous incision was used with a standard deltopectoral approach to place the VRS glenoid baseplate over the anterior rim of the glenoid, which was secured with a central 6.5 × 45 mm nonlocking screw and 4 peripheral 4.75 mm locking screws. A 41 mm glenosphere was impacted onto the taper with maximal offset inferiorly. The humeral bone was deficient from prior osteomyelitis, and 2 cerclage wires were placed to prevent extension of a 2.5 cm cortical defect in the proximal humerus. A 10 × 122 mm cemented humeral prosthesis was implanted in 20° of retroversion with a standard tray and +0 polyethylene. The components were reduced and the subscapularis was repaired with braided nylon sutures.
At 6 months postoperatively, the patient had no pain, a stable implant (Fig. 3), and greatly improved range of motion, with forward elevation to 110° and external rotation to 30°. The implant remains intact and stable 4 years postoperatively.
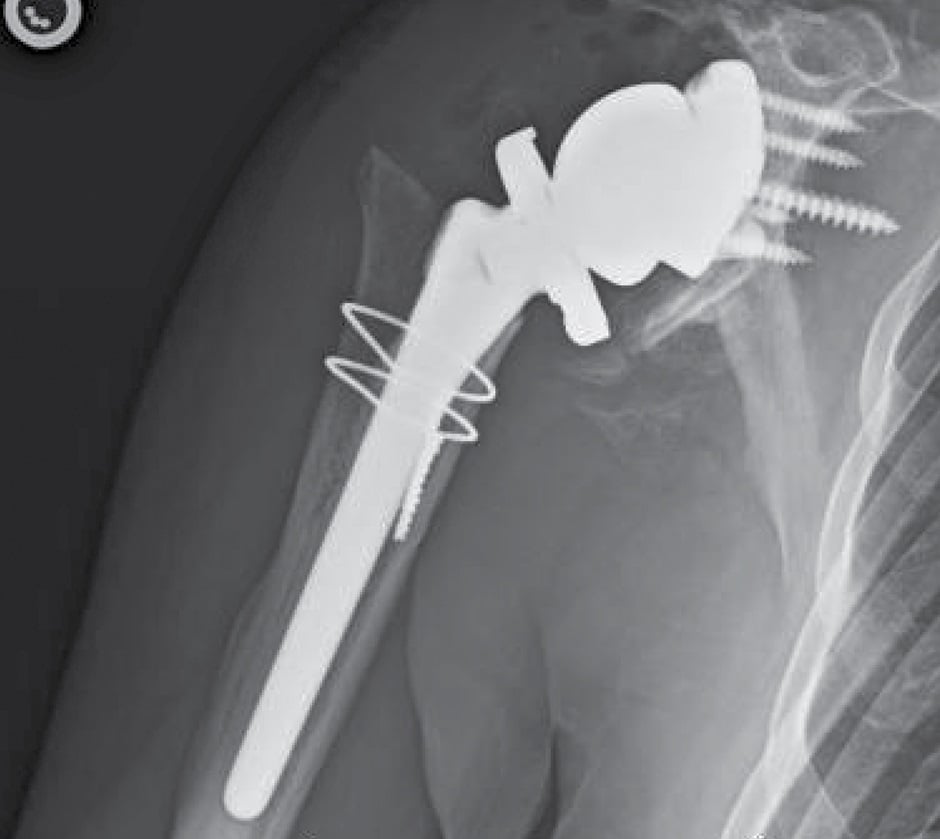
Figure 3: X-rays at 6 months postoperatively show a stable implant.
Discussion
Glenoid deficiency in primary and revision shoulder arthroplasty creates difficulty in positioning the glenoid component in poor bone stock and achieving adequate fixation [1]. Glenoid baseplate fixation failure, bone graft resorption, or inadequate component positioning can lead to increased baseplate stresses and early failure [2]. 3D printing technology has allowed the manufacture of implants that match glenoid bone deformity, which can allow for restoring the joint line, increasing bone–metal contact, stabilizing the baseplate with flanges, and determining preoperatively the ideal length and trajectory of screw fixation. Zimmer Biomet received US Food and Drug Administration 510(k) clearance in 2016 to market the VRS device for use in patients with significant bone loss and is the only implant of this type available in the United States [3].
VRS reconstruction has shown promise in 2 small retrospective case series. Bodendorfer et al reported on 12 shoulders treated with the VRS at average 30 months’ follow-up [4]. Median improvement in American Shoulder and Elbow Surgeons (ASES) scores was 45 points (P < .02), with 20° forward elevation (P < .009), 40° external rotation (P < .014), and 2 spinal levels of internal rotation (P < .002), with no signs of radiographic loosening or complications. Rangarajan et al reported 1-year results of 19 patients treated with the VRS, finding a 47-point improvement in ASES scores (P < .001) and 71° forward elevation (P < .001), with complications in 4 patients [2]. Our case is consistent with outcomes reported in those case series, with 40° improvement in both forward elevation and external rotation and a stable implant 4 years postoperatively, with no reported complications.
References
- Mourad W, Wiater JM, Wiater BP, Martusiewicz A. Baseplate options for reverse total shoulder arthroplasty. Curr Rev Musculoskelet Med. 2020;13(6):769–775.
- Rangarajan R, Blout CK, Patel VV, Bastian SA, Lee BK, Itamura JM. Early results of reverse total shoulder arthroplasty using a patient-matched glenoid implant for severe glenoid bone deficiency. J Shoulder Elbow Surg. 2020;29(7S):S139–S148.
- Dines DM, Gulotta L, Craig EV, Dines JS. Novel solution for massive glenoid defects in shoulder arthroplasty: a patient-specific glenoid vault reconstruction system. Am J Orthop. 2017;46(2):104–108.
- Bodendorfer BM, Loughran GJ, Looney AM, et al. Short-term outcomes of reverse shoulder arthroplasty using a custom baseplate for severe glenoid deficiency. J Shoulder Elbow Surg. 2021;30(5):1060–1067.

