PAO Surgery (Periacetabular Osteotomy)
Summary: This article explains what periacetabular osteotomy (PAO) surgery is, how it works, and when it is recommended for patients with hip dysplasia or other hip alignment conditions. It also outlines the diagnostic imaging used at HSS to plan the procedure, and the recovery process. Readers also learn how hip dysplasia develops, how it affects hip function, and why it can lead to early arthritis if left untreated.

In this article:
What is a periacetabular osteotomy?
A periacetabular osteotomy (PAO) is a surgical treatment for hip dysplasia that is caused by a deformity in the acetabulum, the curved portion of the pelvis that forms the socket of the hip joint. Symptoms of this condition – which may be present from birth, but may only become evident in adolescence or adulthood – generally include hip pain and restricted mobility.
Anatomy of the hip
The hip is a ball-and-socket joint composed of two bones connected by cartilage, ligaments, tendons and muscles:
- the femoral head or tip of the femur (thighbone) is the ball
- the acetabulum, a cup on the side of the pelvis, is the socket
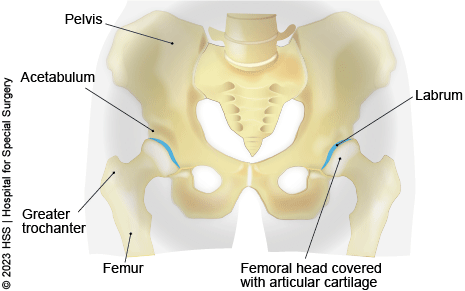
A protective layer of cartilage lines the ball and socket to allow the leg to glide smoothly backward, forward, and sideways. An additional ring of specialized cartilage in the acetabulum called the labrum further protects and stabilizes the joint.
Review of hip dysplasia
In the healthy hip, the upper end of the femur (thigh bone) meets the acetabulum in the pelvis, and the two fit together like a ball and socket, in which the “ball” – the femoral head (top of the femur bone) moves freely in the hip socket.
But in some people, hip dysplasia results when the acetabulum does not develop fully, making it too shallow or otherwise misaligned to adequately contain and support the femoral head. Owing to this misalignment, over time the cartilage and labrum (a soft tissue rim made of fibrous cartilage, which lines the hip socket) can end up bearing the brunt of forces that should be distributed throughout the hip. Left untreated, hip dysplasia can result in early degenerative changes – the wearing down of articular cartilage that covers the hip joint surfaces. These changes mark the beginnings of osteoarthritis, in which the protective labrum and articular cartilage wear away, and bone rubs against bone, leading to pain and restricted mobility. Hip dysplasia is one of the common causes of hip pain and arthritis in patients less than 50 years of age.
Hip dysplasia occurs more frequently in women than in men. Treatment for hip dysplasia ranges from symptomatic relief to surgical correction. In older patients (age 50 and above) with advanced osteoarthritis, total hip replacement may eventually be the best option to alleviate pain and restore mobility. But in younger patients (age 40 and under) in whom joint surface articular cartilage damage has not yet become advanced, a periacetabular osteotomy – in which the surgeon reorients the acetabulum over the femoral head – can offer both symptomatic relief and allow for preservation of the natural hip joint. For patients in their 40s, the most effective treatment is dependent upon the level of hip arthritis.
Diagnosis and presurgical imaging of hip dysplasia
In addition to a thorough physical exam and patient history, orthopedists use X-rays, magnetic resonance imaging (MRI) and, in some cases, three-dimensional (3D) CT scans to confirm a diagnosis of hip dysplasia. The highly sophisticated MRI techniques available at HSS are particularly helpful in providing images that show a clear distinction between bone and cartilage, and in pinpointing the extent of damage to the labrum and other soft tissues, if present.
Imaging can also reveal version deformities in the acetabulum, in which the acetabulum tilts too far forward (anteversion) or too far backward (retroversion).
In addition to serving as a diagnostic tool, we use the 3D CT scans to help plan in advance for anatomical variations in the pelvis they may encounter during surgery. In summary, the diagnosis of hip dysplasia and hip joint stability can be challenging, and it requires careful evaluation of the patient’s symptoms, physical exam and X-rays.
Nonsurgical hip dysplasia treatment
At HSS, many patients with more mild forms of hip dysplasia undergo a trial of nonsurgical treatment with corticosteroid injections and physical therapy. When this approach is successful, the patient is followed with a series of MRIs in order to make sure that there is no progression of damage in the joint.
When is a PAO used to treat hip dysplasia?
For patients with long-standing symptoms or more severe dysplasia, surgery is often recommended at the outset, unless their hip arthritis is too advanced. In milder cases in a person who has reached skeletal maturity (has stopped growing), a PAO may be considered once nonsurgical treatments fail. PAO may also be advised when previous procedures when other procedures, such as a hip arthroscopy, successfully treat injuries to the hip labrum but cannot not address the underlying dysplasia. The decision depends on the patient’s age, lifestyle, goals, and expectations.
How does a PAO work?
In a periacetabular osteotomy, the surgeon makes a series of cuts to the bone to reposition the acetabulum in the pelvis, in order to restore a more normal hip joint anatomy. Screws are then placed in the bones to stabilize this position. During the healing process, new bone forms across the cut surfaces to secure the repositioned acetabulum in the pelvis, establishing proper alignment of the hip joint ball and socket.
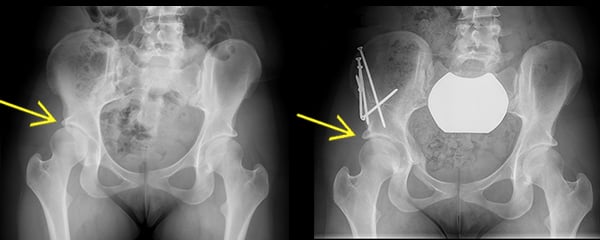
Anterior to posterior X-ray images, before and after a PAO. Left X-ray shows dysplasia of the right hip; the acetabulum is underdeveloped and provides incomplete coverage of the femoral head. Right X-ray shows complete healing of a periacetabular osteotomy, with improved coverage of the femoral head by the acetabulum.
In up to 10% of patients with hip dysplasia, a femoral osteotomy may also be necessary to correct malalignment of the upper part (the head and neck) of the femur. Hip arthroscopy may also be performed along with a PAO in selected patients (for example, to repair a damaged labrum).
Throughout the surgery, X-ray guidance is used and the nerves and muscles that surround and support the hip joint are carefully protected.
What is the recovery time of a PAO?
At HSS, patients who undergo PAO are hospitalized for 2 to 4 days. Physical therapy and instructions on weight-bearing guidelines are initiated before discharge, and crutches must be used for 6 to 8 weeks. Most individuals return to school or work after three months and can resume athletics between 6 to 12 months. If dysplasia affects both hips, the surgeries are performed 4 to 6 months apart.
Periacetabular osteotomy was first developed under the direction of Reinhold Ganz, MD, professor emeritus at the University of Bern in Switzerland. Although the procedure has become more widely used around the world, the HSS Center for Hip Preservation is one of a limited number of centers in the United States where a high volume of these procedures are performed.
In appropriately screened patients who have not developed significant hip joint arthritis, PAOs yield very good results, even up to 20 to 25 years after the procedure.1 Performed by an experienced orthopedic surgeon, PAO has a good safety profile and produces predictable results. If you are considering undergoing a PAO, it’s important to go to a center where the surgeon evaluates a high volume of young hip patients and the team is very familiar with the PAO and other hip preservations surgeries.
Key takeaways
- Periacetabular osteotomy (PAO) is a hip joint preservation surgery that repositions the hip socket to better cover the ball at the top of the femur and relieve pain from hip dysplasia.
- The surgery involves cutting and repositioning the bone to achieve normal alignment; screws are used to stabilize the socket as it heals.
- Hospital stay for a PAO is about 2 to 4 days. Use of crutches lasts 6 to 8 weeks.
- Return to work or school is about 3 months and return to sports about 6 to 12 months.
- Outcomes are excellent when performed by an experienced surgeon who routinely performs PAO.
References
- Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008; 466:1633-1644


