REMOVED - Adult Spinal Deformities: An Overview [rebyline?]
An interview with Frank Schwab, MD
Adult spinal deformity – defined as a deviation in the alignment of the spinal column of more than 10 degrees when viewed from the front, or a loss in normal curvature when viewed from the side – can have a major impact on quality of life. Symptoms may include significant pain and reduced function. Adult spinal deformity refers to a group of conditions in which the spinal column bends abnormally either to the right or to the left. It is commonly associated with a forward-bending posture and increased hunching of the upper back.
Individuals seeking medical attention for adult spinal deformities usually fall into one of five categories – those who:
- Developed a deforming curvature of the spine in childhood or adolescence which has progressed or become more symptomatic in adulthood.
- Develop de novo (new) deformities resulting from injury or “wear and tear” arthritis (osteoarthritis). Injury-related deformities can occur at any time, while those related to osteoarthritis develop in later adulthood and progress with age.
- Have poor bone quality and osteoporosis that leads to the collapse of vertebrae, which are the “building blocks” of the spinal column.
- Have a specific focal problem, such as a degenerative intervertebral disc or spondylolisthesis, a condition in which the affected vertebra slips forward relative to the vertebra below it, both of which can cause a “cascade” of degenerative changes to the spine.
- Have had spinal surgery in the past and, due to ongoing or accelerated wear and tear (or sometimes, due to the position of a previous fusion procedure), develop deformity of the spinal column.
Adult spinal deformities are not uncommon, explains Frank Schwab, MD, Chief of Spine Service at HSS. “In fact, more than half of all individuals over 60 have some level of spinal deformity. As our population ages, that prevalence goes up.” For most people, these changes in spine alignment are minor and do not lead to significant disability. But for some, spinal deformities become progressive, chronic conditions that can have a significant impact on quality of life and function.
“Although patients may experience both pain and disability associated with these deformities, it’s important to differentiate between the two,” Dr. Schwab adds. Pain can sometimes be managed with medication or a nerve block. (This includes pain caused by mechanical issues relating to the integrity or stability of the spine, or caused by nerve irritation that creates radiating pain or altered sensation.) These measures can help the patient live without disabling pain and therefore, increase their function. For other patients, malalignment and poor balance, rather than pain, may be the primary issue that leads to disability. These patients may be unable to stand erect for long periods of time or to walk far because they get exhausted and cannot maintain the posture needed to do so. Pain, malalignment, or a combination of these two issues may prompt the patient to seek additional treatment.
Diagnosis
Multiple factors can contribute to and be involved with adult spinal deformity. This makes the diagnosis more complex than that associated with some other orthopedic conditions. A patient seeking medical attention for hip arthritis, for example, is likely to have a stiff and painful joint. A simple X-ray can usually confirm the diagnosis.
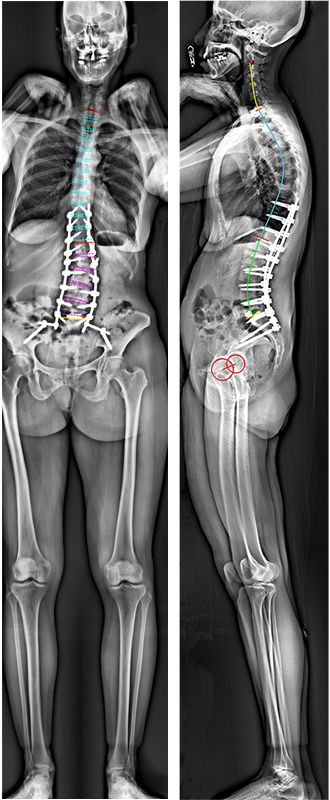
In contrast, the causes, signs and symptoms of adult spinal deformity are more varied, and a clear history of the progression of disability related to the deformity plays an important part in determining treatment. In addition to obtaining a detailed patient history and performing a complete physical exam, spine surgeons at HSS use sophisticated imaging techniques, including X-rays, MRIs, and CT scans, to fully visualize the multiple structures that can be involved with the deformity. [Figures 1. and 2.]
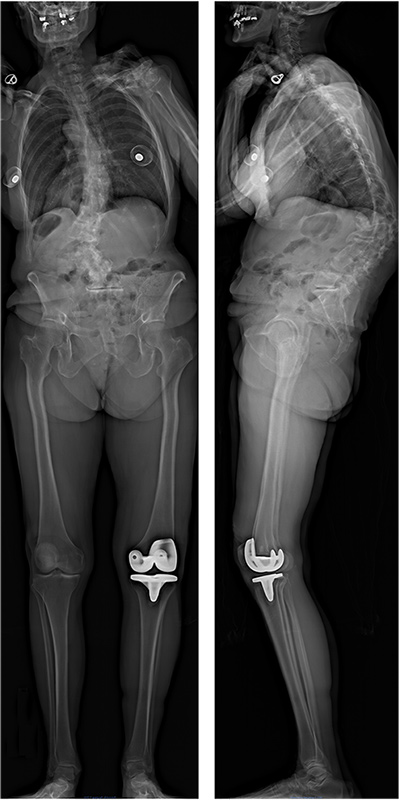
Figure 1. Full-body images are used to assess the alignment of the spine and the recruitment of compensatory mechanisms. The frontal view (left image) reveals a lumbar scoliosis as well as a global malalignment of the trunk toward the left of the patient. The lateral view (right image) reveals a loss of physiological curvatures of the spine compensated by a backward rotation of the pelvis and flexion of the knee.

Figure 2. CT scan images are used to assess the bony elements of the spine. This frontal view of the same patient demonstrates the severity of the scoliosis along with a subluxation of the vertebrae.
Using advanced 3D imaging and computer technology, Dr. Schwab and his colleagues have developed software systems that more clearly define overall spinal alignment, assist in the diagnosis, and facilitate preoperative surgical planning for complex spine surgery. This technology and associated research efforts have led to a definitive classification of adult spinal deformity that has become a clinical standard for spine surgeons worldwide.
Dr. Schwab emphasizes that the effective evaluation of the patient with adult spinal deformity requires an individualized approach. “Experience has shown us that two different patients can have the similar appearing X-rays or MRIs, yet require very different kinds of treatment. We’ve learned which X-ray parameters are important and which ones are not. Also, specific numbers or measurements may be less important to improving function in an individual patient than are relationships between these parameters.”
Dr. Schwab points out that “with so many possible pathologies involved, multiple structures to assess, and individual levels of disability to consider, it can take a fair amount of ‘detective work’ to determine how best to address the specific patient’s deformity.”
Treatment
The goals of surgical treatment of adult spinal deformity are pain relief and improvement of function. Depending on the nature of the deformity, the surgeon may use a variety of techniques to bring the spine back into alignment, secure it as necessary with specialized instrumentation and/or fusion, and remove or adjust spinal structures to relieve nerve pain.
In addition to technology that has enabled better understanding of these conditions and preoperative planning, a number of developments have contributed to the enhanced efficacy of spine surgery, including:
- New ways to stabilize the spine with specialized screws and cables, and ways to promote fusion with biologic agents, bone grafts, and bone cells.
- Techniques that minimize blood loss during surgery.
- Advances in anesthesia that allow for faster recovery and early mobilization.
- Better pain control following surgery.
As with any orthopedic surgery, when determining patient eligibility for procedures to correct adult spinal deformity, the patient’s age and weight are taken into consideration. However, a patient’s level of robustness – which is not necessarily associated with age – may be the most important factor. A frailty index, which assesses a patient’s physiologic reserve and ability to withstand both the surgery and the challenges of recovery, can be a significant predictor of the patient’s length-of-stay at the hospital, potential complications, and prognosis.
Case Example
A 60-year-old woman previously diagnosed with scoliosis developed severe, chronic lower back pain that radiated down both her legs. Her pain restricted her from walking more than two city blocks and significantly impacted her happiness. For relief, she had tried NSAIDs, five epidural steroid injections, and four radiofrequency ablations. However, these all became less effective over time. During a physical exam, the patient had moderate pain in the lumbar spine when flexing, extending, or bending sideways. She did not, however, have pain during straight leg tests, and she had full range of motion, strength, and sensation in her lower extremities.
Radiographs showed scoliosis with a 51-degree Cobb angle in the mid and lower spine, misaligned vertebrae, significant disc collapse, and a loss of normal curvature of the lumbar spine. An MRI showed advanced, degenerative changes throughout the lumbar spine, and a high grade of stenosis. [Figure 3.]
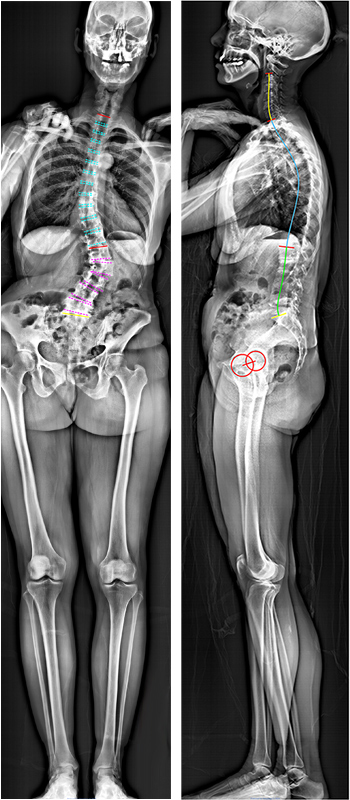
Decompression, stabilization, and restoration of the lordosis (normal curvature of the spine) were accomplished with a wide facet resection and posterior spinal fusion. Pedicle screws were placed bilaterally (on both sides) of each vertebra from T10 to the sacrum and reinforced with bilateral iliac screws. Since her operation, the patient has been very pleased with her posture, and she regained the ability to walk. [Figure 4.]
(Click on image for zoom view)
Figure 3. (Left) Anterior-to-posterior (front-to-back) and, (right) lateral (sideview) full-body images before surgery. The patient exhibited scoliosis measuring 51 degrees, misaligned vertebrae and significant disc collapse. There is a 25-degree loss of lumbar lordosis, compensated with a 32-degree of pelvic retroversion.
Recovery and Outcomes
In recent years, treatment in surgical correction of adult spinal deformity has changed dramatically, with the development of a more individualized and sophisticated approach. So, too, has recovery. Historically, patients undergoing these surgeries were placed in a cast or brace and remained in bed for extended periods of time. After hospitalization, patients were transferred to a separate facility for rehabilitation.
Today, recovery in the hospital is much faster. Moreover, even those patients who undergo surgery involving multiple segments of the spine are out of bed and mobilized soon after surgery. Most patients do not require bracing and return home for rehabilitation following surgery in order to resume their usual routines as quickly possible.
As part of an ongoing commitment to improving patient care, spine surgeons at HSS continue to contribute to a body of knowledge about adult spinal deformity and its treatment. A very important aspect of improving care is understanding the short- and long-term outcome of treatment, particularly as it pertains to quality of life – the thing that matter most to patients. To gain this perspective, patients at HSS are encouraged to enroll in patient-centered prospective outcome registries that track recovery, quality of life issues, and long-term results – data that will help future patients undergoing similar surgeries. (All personal information remains confidential.)
With the many advances in anesthesia, surgical treatment, and postoperative care, there are more treatment options available for adult spinal deformity than ever before. However, Dr. Schwab cautions, it is important for patients and their families to understand that the spine will continue to deteriorate with aging and to understand that the possible need for further surgical treatment does not mean that the initial procedure was a failure.
For example, successfully correcting a deformity due to degenerative disc disease in one section of the spine will not prevent the need for an additional treatment in the future if the disease affects another part of the spine. To further illustrate the point, Dr. Schwab uses the analogy of a patient with heart disease who may require an arterial stent at some point and perhaps another later on, but then still require a pacemaker in the future. In both cases, targeted interventions are used to address specific medical problems as they arise.
Treatment of Adult Spinal Deformity at HSS
For adults with spinal deformity who are considering surgical treatment, Dr. Schwab advises choosing an institution where many such procedures are performed yearly, such as HSS. He also cites the hospital’s team approach as a key element in providing optimal care. “Between 5 to 10 people are involved in the treatment of the patient in the operating room and postoperatively. These include nurses, anesthesiologists and intensivists, as well as physicians from the Department of Medicine and the Pain Management Division.” Patients who require revision surgeries for adult spinal deformity are also seen frequently at HSS – what might seem rare at other institutions is commonly managed at HSS.
If you would like more information about treatment of adult spinal deformity at HSS, please visit the Physician Referral Service or call 1.877.606.1555.
Posted: 7/20/2016
Summary by Nancy Novick