Osgood-Schlatter Disease
Osgood-Schlatter is a common overuse condition of the knee in growing children who are physically active. It is a temporary condition that may come and go throughout a child's growth period.

What is Osgood-Schlatter disease?
Osgood-Schlatter is an overuse condition in which pain is isolated to a bump located just below the front of the knee.
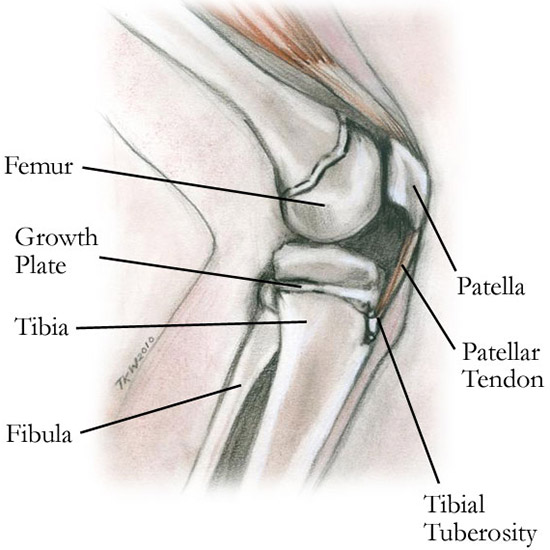
Sketch of a lateral view (from the side) of a child's knee.
(Created by Tonnie Warfield, RN)
This bony prominence, known as the tibial tubercle (or tibial tuberosity), is located where the patellar tendon meets the upper end of the tibia (shinbone). The condition affects physically active, growing children and teenagers (usually aged 9 to 13 years).
The inclusion of the word “disease” is actually misleading, since this is not truly a “disease” but rather an overuse syndrome. It is common and temporary, and children usually outgrow it without any lingering problems. The condition was named after two surgeons, Robert Bayley Osgood of the United States and Carl B. Schlatter of Switzerland who, independent of each other's work, were the first physicians to describe it.
What are the symptoms of Osgood-Schlatter?
Symptoms include pain and swelling over the tibial tubercle that worsens with activity and improves with rest. Usually, there is pain with kneeling and any activity in which the knee is bent or completely extended, such as running or squatting. In most cases, only one knee is affected.
What causes Osgood-Schlatter?
With repetitive activities, the patellar tendon in the knee becomes irritated and inflamed at its point of attachment to the tibial tubercle. This repetitive activity, combined with accelerated growth of a child’s bone, causes traction at the tendinous insertion. This stimulates the formation of a bony prominence or “bump” below the knee.

Inflamed bump over the tibial tubercle, just under the knee.
What are the risk factors for Osgood-Schlatter?
An imbalance of muscle forces, from the quadriceps in front to the hamstrings behind the thigh, can occur from overuse in sports and from growth. This imbalance may increase the risk for Osgood-Schlatter disease. A review of imaging of patients’ knees demonstrates that the slope of the surface of the tibial side of the knee joint tends to be steeper in patients that have Osgood-Schlatter disease, suggesting there may be anatomical risk factors. Research at HSS is currently underway to determine whether young patients with Osgood-Schlatter disease may also be susceptible to other knee injuries, such as ACL tears.
How do you prevent Osgood-Schlatter?
While Osgood-Schlatter may not be completely preventable in highly active children, especially those engaged in impact sports or dance, diligent stretching of the quadriceps and hamstring muscles may diminish the severity of symptoms. Increasing strength and flexibility in the thigh muscles helps keep growing athletes agile and less susceptible to this overuse injury. As soon as any symptoms ensue, icing the affected area after activity will diminish the inflammation.
How is Osgood-Schlatter diagnosed?
This condition is best treated by a pediatric orthopedic specialist who can diagnose and manage the condition. The doctor will want to know the duration of symptoms and what aggravates and alleviates the pain. Sometimes X-rays are necessary. (Find a pediatric orthopedist at HSS who treats Osgood-Schlatter.)
What is the treatment for Osgood-Schlatter disease?
The treatment goal is to keep the child active, but pain free. Sometimes rest or modifying athletic activity is necessary to reduce pain. Wearing a strap just below the kneecap while the child is active and icing the bony prominence after activity may alleviate symptoms. The pediatric orthopedist will help sort out which activities are appropriate to continue, and they may prescribe physical therapy to establish a stretching and strengthening regimen. If the pain does not go away, sometimes a brace is recommended along with physical therapy. Surgery to remove the painful bony prominence is performed only rarely for patients who do not improve with non-operative interventions.
What is the recovery time for Osgood-Schlatter?
For competitive athletes, modifying training regimens for two to three months may be necessary. During the healing phase, ibuprofen (Motrin or Advil) may help reduce swelling and pain. Ice can help as well when applied to the painful area after exercise. Osgood-Schlatter disease usually resolves within 6 to 18 months.
Though the bony prominence may persist when the pain is gone, activities may be resumed gradually. Once a person completes their growth cycle and the growth plates around the knee close, Osgood-Schlatter resolves without recurrence.
Osgood-Schlatter Disease Success Stories
Updated: 10/13/2023
Reviewed and updated by John S. Blanco, MD; Emily R. Dodwell, MD, MPH, FRCSC; Shevaun Mackie Doyle, MD; Peter D. Fabricant, MD, MPH; Daniel W. Green, MD, MS, FAAP, FACS; and David M. Scher, MD

