A 9-Year-Old Boy with Anterior Knee Pain and Genu Valgum Treated with Implant-Mediated Guided Growth
From Grand Rounds from HSS: Management of Complex Cases | Volume 13, Issue 2
Case Report
Following a patellar dislocation of the left knee, a 9-year-old skeletally immature boy was diagnosed with genu valgum accompanied by recurrent bilateral patellar instability. His right knee was significantly less symptomatic. Bilateral X-rays and long-standing EOS radiographs demonstrated bilateral genu valgum and lateral patellar subluxation, with increased patellar tilt also noted (Figure 1). On clinical examination, there was patellar apprehension, full range of motion, and mild J-sign bilaterally.

Figure 1: Preoperative EOS radiograph of 9-year-old boy demonstrating bilateral genu valgum.
The patient was recommended for and underwent bilateral hemiepiphysiodesis with hinged tension-band plates to correct lower extremity malalignment contributing to his patellar instability. Additionally, simultaneous left-sided medial patellofemoral ligament (MPFL) reconstruction with hamstring (gracilis) tendon allograft and lateral retinacular release was performed to improve patellar tracking (Figure 2).
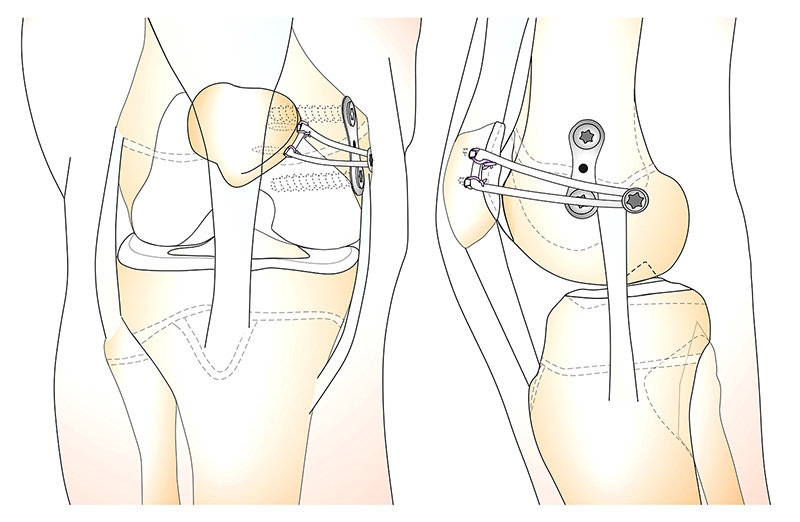
Figure 2: Simultaneous distal femur hemiepiphysiodesis and MPFL reconstruction [6].
Hemiepiphysiodesis begins with an incision adjacent to the medial epicondyle and adductor tubercle. A guidewire is placed behind the medial epicondyle and angulated distally away from the growth plate. The position is confirmed radiographically, referencing Schottle’s radiographic landmarks. A pouch is then created under the first layer of the medial retinaculum from the patellar incision to the medial retinacular incision. After the MPFL epiphyseal insertion point is confirmed, the graft can be placed into the distal femur. Then, a guidewire is placed 1 cm anterior to the MPFL insertion site to confirm the epiphyseal screw used for the hinged tension-band plate is properly placed. After insertion of the epiphyseal screw, the metaphyseal portion of the plate is brought beneath the vastus medialis oblique (VMO) on the metaphysis and secured by a guidewire. Once the position is confirmed on X-ray, the plate is secured with a screw. MPFL reconstruction involves the attachment of the 2 free ends of the hamstring gracilis allograft to the patella.
Nine months postoperatively, X-rays showed correction of the patient’s genu valgum (Figure 3). He was subsequently recommended for removal of hinge plates and for concurrent right-sided MPFL reconstruction with hamstring allograft and lateral retinacular release due to a symptomatic right knee (history of multiple patella dislocations/subluxation and persistent patellofemoral instability). The patient will be followed postoperatively and displays no complications in the left knee following the initial surgery.
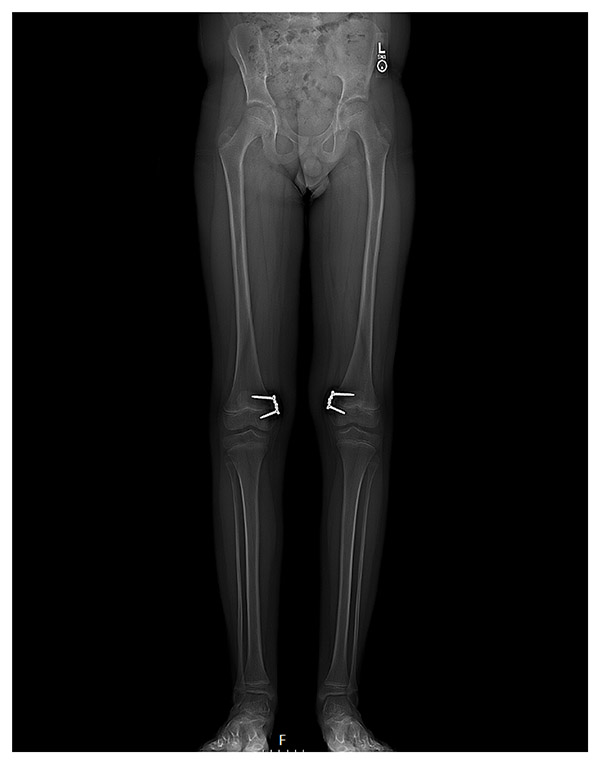
Figure 3: 9 months postoperative EOS radiograph showing correction of genu valgum, before hardware removal.
Discussion
Lower-extremity coronal plane malalignment appearing as genu valgum can lead to patellofemoral instability (PFI). An elevated quadriceps (Q) angle imposes a laterally directed vector on the patella, increasing the tibial tubercle-trochlear groove (TT-TG) distance and resulting in PFI [1].
Implant-mediated guided growth (IMGG) is considered in the setting of patellofemoral instability if pathological genu valgum is present and the patient has more than 2 years of growth remaining. Contraindications for IMGG include skeletal maturity, physeal bar growth arrest, and multiplanar deformity including genu valgum with severe femoral anteversion. IMGG is commonly used to correct coronal plane angular deformities and may be performed simultaneously with MPFL reconstruction to address PFI. IMGG using hinged tension-band plates allows for future growth while correcting lower-extremity deformities [2–5].
This case highlights the successful use of IMGG and MPFL reconstruction to simultaneously treat bilateral genu valgum and PFI. Studies have demonstrated performing simultaneous MPFL reconstruction and IMGG is a safe and viable option for pediatric patients experiencing PFI induced by coronal plane malalignment [5–7].
Authors
Chief of the Pediatric Orthopedic Surgery Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery
Emilie Lijesen, BS
Research Assistant
Hospital for Special Surgery
Shae K. Simpson, BS
Research Assistant
Hospital for Special Surgery
References
- Accadbled F, Kerdoncuff A, Hidalgo Perea S, Green DW. Failure of isolated medial patellofemoral ligament reconstruction in children: Risk factors and management. J Child Orthop. 2023;17(1):34-39. doi: 10.1177/18632521221149055.
- Braga SR, Santili C, Rodrigues NVM, Soni JF, Green DW. Growth modulation for angular knee deformities: a practical guideline. Curr Opin Pediatr. 2023;35(1):110-117. doi: 10.1097/MOP.0000000000001183.
- Lin KM, Fabricant PD. CORR Synthesis: Can guided growth for angular deformity correction be applied to management of pediatric patellofemoral instability? Clin Orthop Relat Res. 2020;478(10):2231-2238. doi: 10.1097/CORR.0000000000001311.
- Lin KM, Thacher RR, Apostolakos JM, et al. Implant-mediated guided growth for coronal plane angular deformity in the pediatric patient with patellofemoral instability. Arthrosc Tech. 2021;10(3):e913-e924. doi: 10.1016/j.eats.2020.11.012.
- Parikh SN, Redman C, Gopinathan NR. Simultaneous treatment for patellar instability and genu valgum in skeletally immature patients: a preliminary study. J Pediatr Orthop B. 2019;28(2):132-138. doi: 10.1097/BPB.0000000000000546.
- Bram JT, Tracey OC, Lijesen E, et al. Simultaneous MPFL reconstruction and guided growth result in low rates of recurrent patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2024;32(5):1105-1112. doi: 10.1002/ksa.12134.
- Ellsworth BK, Aitchison AH, Fabricant PD, Green DW. Use of implant-mediated guided growth with tension band plate in skeletally immature patients with knee pathology: a retrospective review. HSS J. 2022;18(3):399-407. doi: 10.1177/15563316211010720.


