Chronic Enterovirus Infection Manifesting as Diffuse Myalgias and Arthralgias in a 67-Year-Old Woman Receiving Obinutuzumab
From Grand Rounds from HSS: Management of Complex Cases | Volume 12, Issue 3
Case Report
A 67-year-old woman with chronic lymphocytic leukemia (CLL) and iatrogenic hypogammaglobulinemia was hospitalized for evaluation of fever of unknown origin. She was initially diagnosed with CLL (Rai stage I) 7 years prior and managed with observation. One year prior to hospitalization she developed worsening fatigue, lymphocytosis, and lymphadenopathy, for which she received obinutuzumab and venetoclax; 3 months prior she developed low-grade fever, frontal headache, diffuse myalgias, and polyarthralgias after travelling. Although she tested negative for tickborne illness, she was treated with 2 courses of doxycycline that did not reduce symptoms. Having been evaluated by rheumatology as an outpatient 4 weeks prior, she was empirically treated with prednisone 40 mg daily. She continued to experience fevers, headache, myalgias, and arthralgias without sicca symptoms. Worsening transaminitis prompted a liver biopsy, which demonstrated an acute hepatitis with many necro-inflammatory foci (Fig. 1). She was subsequently admitted for further evaluation.
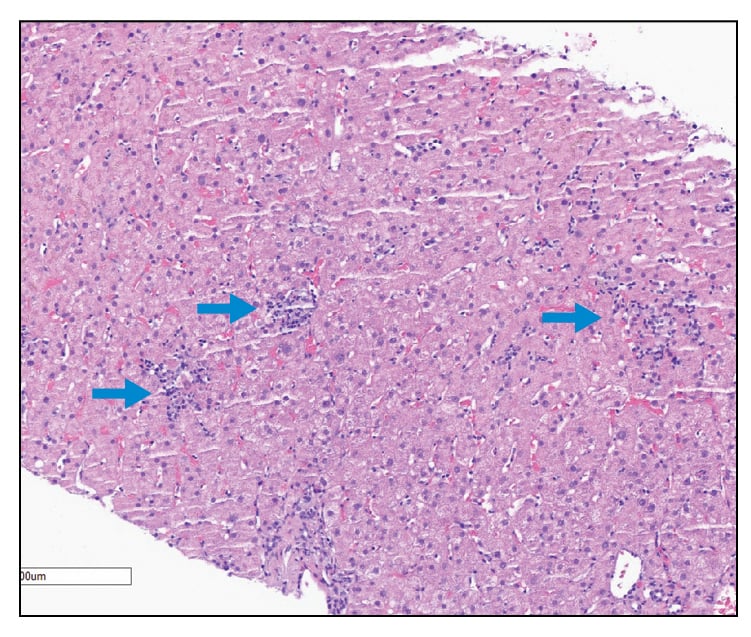
Figure 1: Liver biopsy demonstrating an acute hepatitis with spotty necro-inflammatory foci (blue arrows).
On presentation she had a temperature of 37.3°C, heart rate of 73 beats per minute, blood pressure of 105/62 mmHg, respiratory rate of 16 breaths per minute, and oxygen saturation 100% on ambient air. Musculoskeletal examination was notable for tenderness of the forearms and legs and the absence of synovitis.
Laboratory workup showed normal erythrocyte sedimentation rate and C-reactive protein levels, positive for anti-Ro antibodies (6.6; normal < 1.0), and negative for antinuclear antibody, double-stranded DNA, anti-La, anti-Smith (Sm)/ribonucleic protein (RNP), rheumatoid factor, anti-cyclic citrullinated peptide (anti-CCP), and antineutrophil cytoplasmic antibody (ANCA). Creatine kinase levels were normal. Serum aspartate aminotransferase (AST) level was 2810 U/L (reference ≤ 34), and alanine transaminase (ALT) level was 2698 U/L (reference range 10-49). She was noted to have hypogammaglobulinemia (immunoglobulin G [IgG] 499 [reference range 610-1,717], IgM <10 [reference range 35-242], and IgA 22 [reference range 85-499]), a finding not significantly changed from 1 month prior to the onset of symptoms.
Positron emission tomography–computed tomography (PET-CT) scanning did not demonstrate 18F-fluorodeoxyglucose (FDG)-avid lymphadenopathy or evidence of occult malignancy. Magnetic resonance imaging (MRI) of the brain demonstrated bilateral convexity pachymeningeal thickening and enhancement (Fig. 2). Cerebrospinal fluid testing demonstrated a white blood cell count of 42/mm3 (91% lymphocytes), a red blood cell count of 8/mm3, and normal levels of glucose and protein. Bacterial, acid-fast bacilli, and fungal cultures were negative. However, both respiratory and cerebrospinal fluid PCR testing demonstrated the presence of enterovirus RNA. She received 2 g/kg intravenous immunoglobulin (IVIG) for treatment of chronic enterovirus infection, with outpatient monitoring of IgG levels every 6 weeks and IVIG replacement if less than 650 mg/dL. Within 3 months of discharge, she had symptomatic resolution and normalization of liver enzymes.
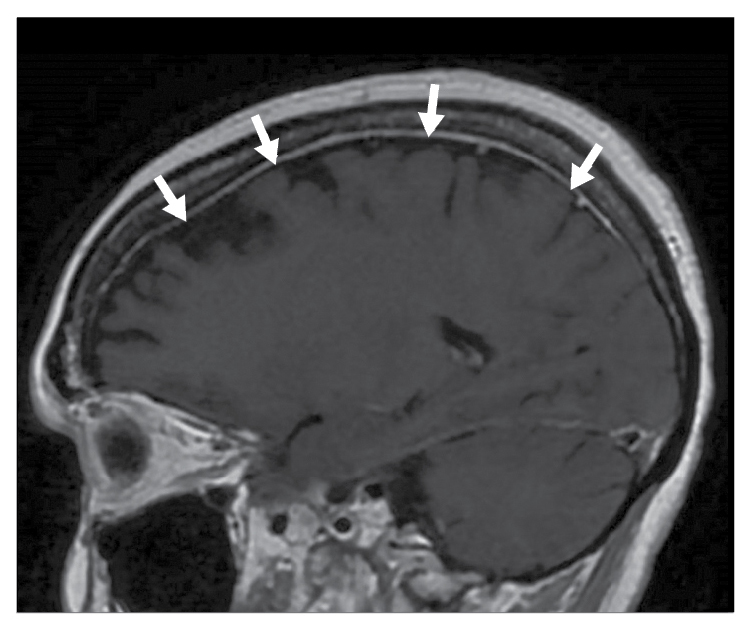
Figure 2: A sagittal T1-weighted image post intravenous (IV) gadolinium demonstrating mild bilateral convexity pachymeningeal thickening and enhancement (white arrows).
Discussion
Although acute viral infections commonly present with myalgias and arthritis or arthralgias, they are typically self-limited illnesses in immunocompetent patients. Chronic enterovirus infection is rare but can be seen in patients with hereditary or acquired deficiencies in humoral immunity that may present as chronic meningoencephalitis, dermatomyositis-like syndrome, or acute hepatitis [1]. Obinutuzumab, an anti-CD20 monoclonal antibody that mediates B-cell lysis, is approved for the treatment of CLL and other hematologic malignancies; its use is also being evaluated for rheumatic diseases such as systemic lupus erythematosus [2]. This patient presented with a protracted and disseminated viral illness with chronic myalgias and arthralgias, presumably as a complication of her B cell-depleting therapy.
Several case reports have identified the potential efficacy of IVIG for the treatment of disseminated enterovirus infection in patients with deficiencies in humoral immunity [3, 4]. This patient similarly experienced symptom resolution after the initiation of IVIG.
This case highlights the importance of maintaining a broad differential diagnosis for a patient with musculoskeletal complaints, including infectious etiologies, particularly in those who are on immunosuppressive therapy.
References
- Grammatikos A, Donati M, Johnston SL, Gompels MM. Peripheral B cell deficiency and predisposition to viral infections: the paradigm of immune deficiencies. Front Immunol. 2021;12:731643.
- Furie RA, Aroca G, Cascino MD, et al. B-cell depletion with obinutuzumab for the treatment of proliferative lupus nephritis: a randomised, double-blind, placebo-controlled trial. Ann Rheum Dis. 2022;81(1):100-107.
- Anderson SM, Gold D, Olson G, Pisano J. Chronic aseptic meningitis caused by enterovirus in a humorally immunosuppressed adult patient presenting with sensorineural hearing loss: a case report. BMC Infectious Diseases. 2022;22(1):16.
- Grisariu S, Vaxman I, Gatt M, et al. Enteroviral infection in patients treated with rituximab for non-Hodgkin lymphoma: a case series and review of the literature. Hematol Oncol. 2017;35(4):591-598.

