The Use of Novel Technologies in Coronal Plane Correction in a 72-Year-Old Man
From Grand Rounds from HSS: Management of Complex Cases | Volume 12, Issue 2
Case Report
A 72-year-old man with a history of familial adenomatous polyposis (FAP) presented with debilitating right-leaning posture, causing an inability to stand and ambulate upright. He noted a worsening truncal shift 9 years prior, after abdominal surgeries for a complicated visceral infection. He had no neurologic symptoms and underwent physical therapy without improvement.
Physical examination was notable for a significant, though flexible, right truncal shift. He had global 5/5 strength with grossly intact sensation, symmetric reflexes, and no long tract findings.
Full-length standing radiographs demonstrated coronal imbalance (CI) of 113 mm (distance from the C7 plumb line to the central sacral vertical line) and a left thoracolumbar curve of 46° (27.3° supine) (Fig. 1). Relevant pelvic parameters were T1 pelvic angle of 47°, pelvic incidence of 54°, lumbar lordosis of 12.9°(44.5° supine), and pelvic tilt of 33°. There was no leg length discrepancy. Magnetic resonance imaging (MRI) showed severe central canal stenosis at L3–L4; computed tomography (CT) scanning was notable for an average Hounsfield units of 157 (normal bone mineral density) [2].
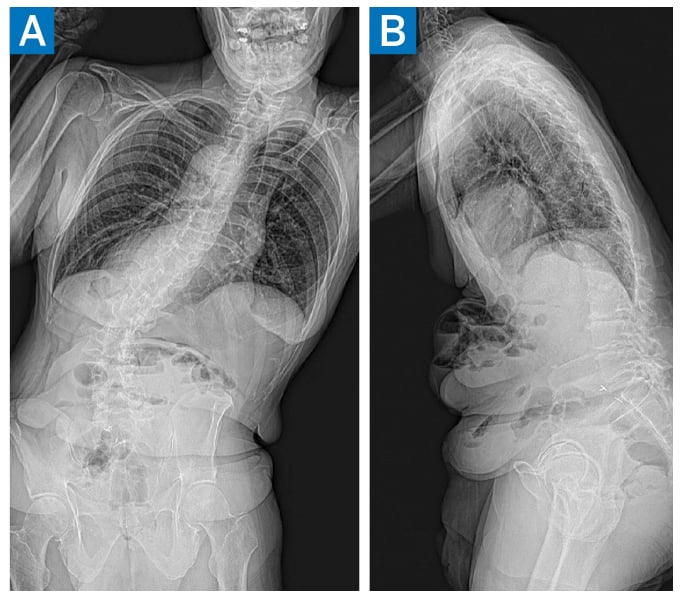
Figure 1: Preoperative anteroposterior (AP) (A) and lateral (B) standing radiographs demonstrating multilevel spondylosis/degenerative scoliosis.
Given symptom progression and worsening disability, the patient underwent T10-to-pelvis instrumented fusion with L3–L4 decompression.
A midline posterior approach was used, extending from T10 to the sacrum. The T8 and T9 spinous processes were exposed to allow for proximal tethering. Pedicle screws were placed bilaterally from T10 to S1 using a combination of freehand technique and an optical topographic surgical navigation system (7D Surgical). System registration was performed via reference array attachment to the exposed bony elements, on which an overhead light source was shined. Stereoscopic cameras recorded the distortion of the light rays, from which a topographic map was generated and synced with a preoperative CT scan. The reference array was adjusted for cephalad levels, as needed. Bilateral pelvic fixation was also performed using this system.
Inferior facetectomies were performed at every level, the interspinous ligaments were removed from L1–S1, and a central decompression was performed at L3–L4. Reduction of the deformity was then performed. First, the lordosis was locked in using an appropriately contoured rod placed on the concave side. Next, a similarly contoured rod was seated loosely on the right side, and an accessory rod was placed in an additional right pelvic screw. The curve convexity was then reduced via distraction performed against the main rod and a rod gripper. Intraoperative X-rays demonstrated appropriate correction.
Burr holes were made in the spinous processes of T8 and T9, and 2 Nile posterior spinal tethers (Stryker) were passed and secured to the rods. Demineralized bone matrix was placed around these tethers to reinforce the construct. Final tightening, fusion bed preparation, and closure were then performed in standard fashion.
An enhanced recovery pathway [3] was enacted, and the patient was discharged home on postoperative day 4. At 6-week follow up, he said he could walk nearly 20 blocks and stand up for more than 10 minutes, the best he had achieved in years. At 3-month follow up, he noted minimal back pain and was comfortably taking long walks outdoors. X-rays demonstrated maintained alignment (Fig. 2).
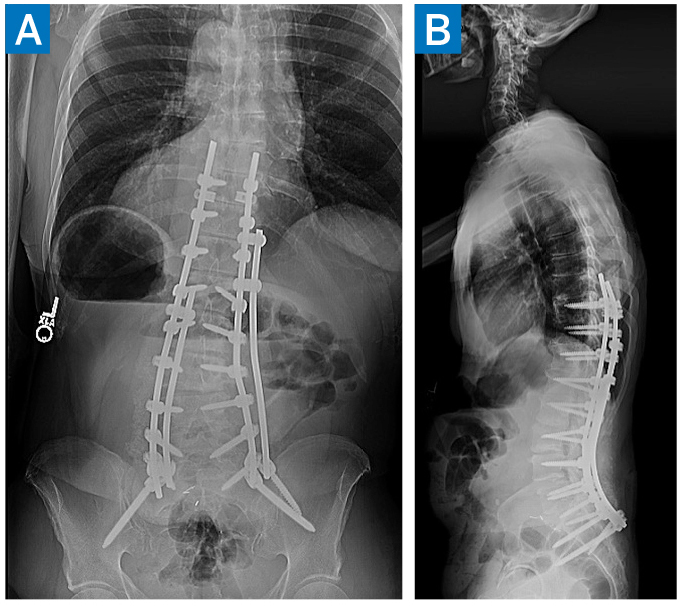
Figure 2: 3-month postoperative AP (A) and lateral (B) X-rays demonstrating maintained deformity correction.
Discussion
Adult spinal deformity is a complex pathology affecting older adults. Significant CI in an older patient may require 3-column osteotomy or interbody technique in the setting of poor bone quality. To mitigate potential surgical risk in this case, we used optical navigation, accessory rods, and proximal ligamentous augmentation to address severe coronal malalignment [1].
The 7D surgical system is an example of “machine vision,” using software, video, and a light projector to generate a topographic map for navigation and for rapid re-registration of adjacent levels without intraoperative imaging (Fig. 3) [4]. Also, the “kickstand rod” technique allows for coronal plane correction through the lumbosacral junction and lumbar posterior column osteotomies; studies have shown its corrective power and low complication profile [1,5]. Proximal spinous process tethering has gained attention in preventing proximal junctional kyphosis. Biomechanical analysis has shown that tethers reduce the flexion moment at the proximal construct and may more widely disperse dynamic loads across the cephalad levels, though further study is warranted [6].
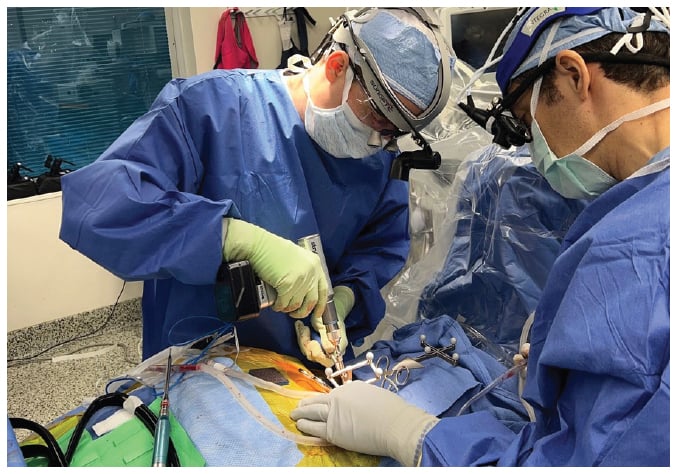
Figure 3: 7D Surgical Navigation System consists of an overhead light embedded with navigation optics, plus standard lighting that contains infrared cameras that may track instruments and project for machine vision.
References
- Makhni MC, Zhang Y, Park PJ, et al. The “kickstand rod” technique for correction of coronal imbalance in patients with adult spinal deformity: initial case series. J Neurosurg Spine. 2019;1–8. doi:10.3171/2019.9.SPINE19389.
- Sardar ZM, Coury JR, Cerpa M, et al. Best practice guidelines for assessment and management of osteoporosis in adult patients undergoing elective spinal reconstruction. Spine (Phila Pa 1976). 2022;47(2):128–135. doi:10.1097/ BRS.0000000000004268.
- Kim HJ, Steinhaus M, Punyala A, et al. Enhanced recovery pathway in adult patients undergoing thoracolumbar deformity surgery. Spine J. 2021;21(5):753–764. doi:10.1016/j. spinee.2021.01.003.
- Kalfas IH. Machine vision navigation in spine surgery. Front Surg. 2021;8:640554. doi:10.3389/ fsurg.2021.640554.
- Redaelli A, Langella F, Dziubak M, et al. Useful and innovative methods for the treatment of postoperative coronal malalignment in adult scoliosis: the “kickstand rod” and “tie rod” procedures. Eur Spine J. 2020;29(4):849–859. doi:10.1007/s00586-019-06285-7.
- Mar DE, Clary SJ, Burton DC, mciff TE. Biomechanics of prophylactic tethering for proximal junctional kyphosis: characterization of spinous process tether pretensioning and pull-out force. Spine Deform. 2019;7(2):191–196. doi:10.1016/j.jspd.2018.06.017.


