Triple Nerve Transfer and Long Nerve Grafts Restore Function in a Devastating Brachial Plexus Injury
From Grand Rounds from HSS: Management of Complex Cases | Volume 9, Issue 1
Case Report
An 18-year-old left-handed woman presented with right upper extremity weakness and numbness 6 weeks after a motor vehicle collision (she had hit a tree as an unrestrained driver). She could not fully move her right shoulder, flex or extend her elbow, or extend her wrist and digits.
Clinical examination demonstrated complete palsy of her supraspinatus, infraspinatus, deltoid, biceps, brachialis, triceps, wrist extensors, and digital extensors. She had no Horner syndrome, no scapular winging, and no sensation in the C5 and C6 dermatomes. The patient was diagnosed with a complete upper trunk and partial C7 brachial plexus palsy.
Electrodiagnostic (EDX) studies at 3 months post-injury demonstrated no voluntary motor unit action potentials (MUAPs) in the supraspinatus, infraspinatus, deltoid, triceps, biceps, brachioradialis, or wrist extensors. EDX findings were consistent with a predominately postganglionic and severe brachial plexopathy of C5 through C7. A multidisciplinary brachial plexus case conference was held to discuss findings of all preoperative studies. Given her lack of spontaneous recovery, we recommended surgical reconstruction to restore shoulder and elbow function, and the patient agreed.
The patient underwent surgery at 4 months post-injury. She was positioned supine with the neck, right upper extremity, and both lower extremities prepared and draped. Two teams operated simultaneously, using multiple approaches to the right supra- and infraclavicular brachial plexus and right sural nerve area (posterior calf to the lateral ankle).
In the supraclavicular region, a large upper trunk neuroma was excised and thin slices of the C5 and C6 root contributions sent for frozen section histologic analysis. The C6 nerve root demonstrated well-defined myelinated axons in more than two-thirds of the cut section, while the C5 root had less than 50% axonal viability. The C6 root demonstrated intact axonal continuity by somatosensory evoked potential (SSEP), while the C5 root demonstrated no response. Based on these data, we elected to use the C6 root for nerve grafting.
In the infraclavicular region, the axillary, musculocutaneous, median, ulnar, radial, pectoral, and thoracodorsal nerves were identified and neurolysed. A double fascicular nerve transfer was performed to restore elbow flexion by first isolating the motor branches to the biceps and brachialis and dividing these from the parent musculocutaneous nerve. A double Oberlin transfer to the arm was used to restore elbow function [3]. Microscopic dissection and electrical stimulation were used to identify individual nerve fascicles of the median and ulnar nerves, which control wrist flexion and forearm pronation. These fascicles were divided distally, with enough length to allow rotation and microscopic nerve suture to the biceps and brachialis motor branches [3] (Fig. 1).
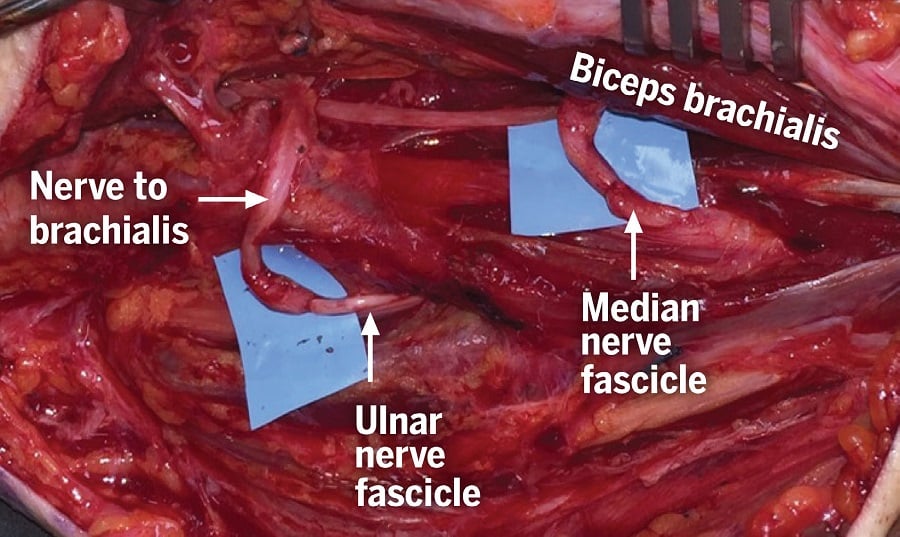
Figure 1: A double Oberlin transfer to the arm to restore elbow function. Nerve fascicles from the median and ulnar nerves are transferred to the nerves to the biceps and brachialis, respectively.
Simultaneously, the supraclavicular team had prepared the distal branches of the spinal accessory nerve for microscopic transfer to the suprascapular nerve, which had been divided from the injured upper trunk. This transfer was performed to restore shoulder abduction and external rotation via the rotator cuff (Fig. 2). Lastly, 45 cm of sural nerve graft was harvested, and a 15-cm cable graft was interposed between the C6 nerve root proximally and the axillary nerve distally. All grafts and transfers were sewn with 8-0 and 9-0 nylon sutures and reinforced with fibrin glue. Given its partial involvement, the C7 nerve root was kept intact in anticipation of possible spontaneous recovery of elbow, wrist, and digit extension.
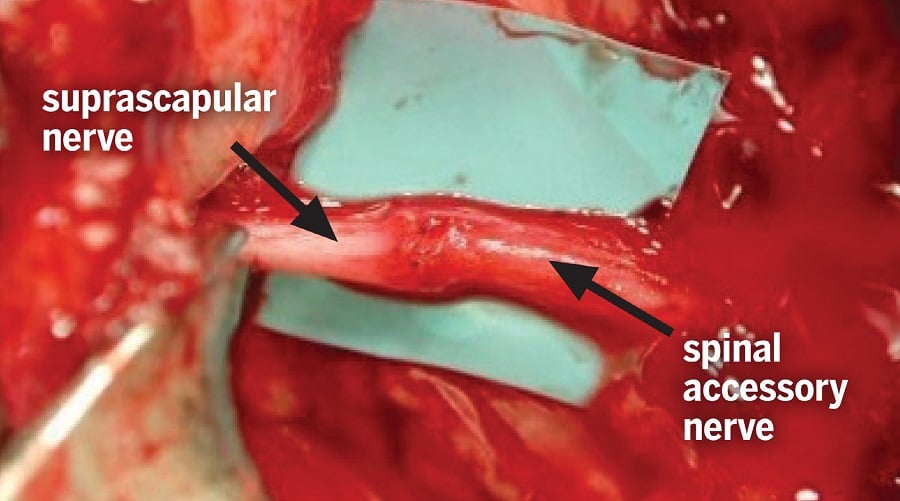
Figure 2: Spinal accessory nerve transfer to the suprascapular nerve to restore shoulder function.
Postoperatively, the patient started to recover active elbow flexion at 4 months, elbow extension and shoulder function at 6 months, and wrist and digit extension at 9 months. EDX at 9 months showed evidence of significant axonal regeneration (decreased recruitment with nascent potentials or di- or triphasic configurations) to the extensor carpi radialis, triceps lateral and medial heads, middle and posterior deltoid, brachioradialis, biceps, brachialis, flexor carpi radialis, pronator teres, supraspinatus, and infraspinatus. There was also axonal regeneration to the extensor pollicis longus and anterior deltoid, but this was limited (discrete recruitment with nascent potentials). At her most recent follow-up visit 6 years after surgery, she had M5 strength in shoulder abduction (100°), external rotation (50°), elbow flexion (150°), finger flexion (full), wrist extension (60°) (Fig. 3), and the intrinsic muscles. She has excellent upper extremity function and has returned to a full workout regimen.
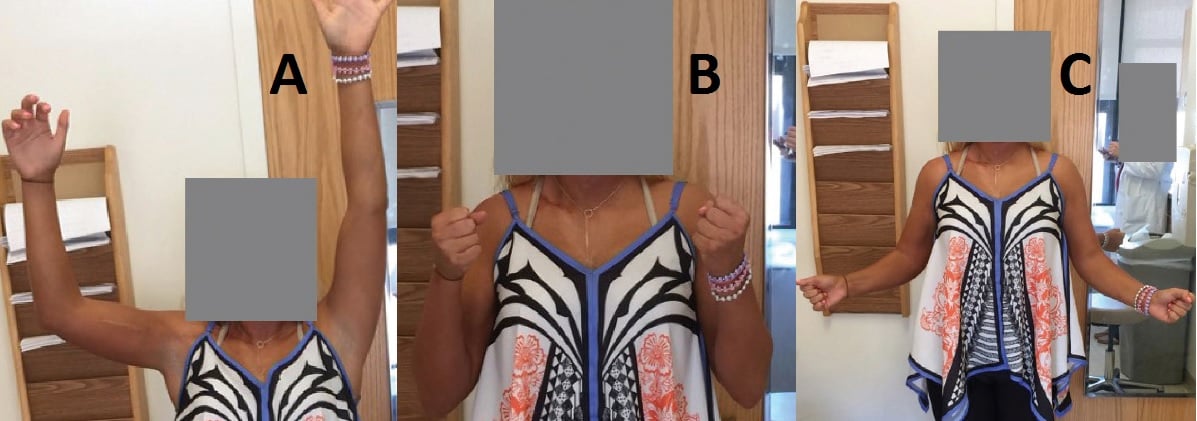
Figure 3: The patient showed significantly improved active range of motion at 6 years postoperatively, abducting the shoulder to 100° (A), flexing the elbow to 150° (B), and externally rotating the shoulder symmetrically (C).
Discussion
Traumatic brachial plexus injuries require comprehensive preoperative evaluation and planning, including meticulous physical examination and EDX, to determine the optimal strategies for neurolysis, nerve transfer, and grafting [1]. This case highlights the transfer of intact portions of pure motor nerves including the spinal accessory nerve and selective motor fascicles of the median and ulnar nerves [2, 3] to restore shoulder abduction, external rotation, and elbow flexion. The case also illustrates the successful use of long nerve grafts to restore axillary nerve function, a prior technique that had been largely abandoned but that HSS physicians have resurrected and refined [4]
References
- Brophy R, Wolfe S. Planning brachial plexus surgery: treatment options and priorities. Hand Clin. 2005;21:47–54.
- Lee SK, Wolfe SW. Nerve transfers for the upper extremity: new horizons in nerve reconstruction. J Am Acad Orthop Surg. 2012;20:506–517.
- Mackinnon S, Novak C, Myckatyn T, Tung T. Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. J Hand Surg Am. 2005;30:978–985.
- Wolfe SW, Johnsen PH, Lee SK, Feinberg JH. Longnerve grafts and nerve transfers demonstrate comparable outcomes for axillary nerve injuries. J Hand Surg Am. 2014;39:1351–1357.





