A 16-Year-Old Female Lacrosse Player with Failed Tibial Tubercle Osteotomy (TTO) Treated with Arthroscopy and Revision TTO
From Grand Rounds from HSS: Management of Complex Cases | Volume 13, Issue 2
Case Report
A 16-year-old female lacrosse player presented to the clinic with left knee pain. She reported no traumatic injuries and said she had suffered 2 previous noncontact lateral dislocations: at age 11 and at age 13. A year prior, she had undergone a tibial tubercle osteotomy (TTO) combined with a medial patellofemoral ligament (MPFL) reconstruction and particulated cartilage implant to the patella and trochlea. The patient reported quadriceps weakness with difficulty ambulating. Physical examination revealed anterior knee crepitus with range of motion, 3/5 quadriceps strength, and tenderness to palpation over the tibial tubercle. Computed tomography (CT), magnetic resonance imaging (MRI), and X-ray of the prior TTO revealed fragmentation of the tibial tubercle shingle and patella alta, as indicated by a Caton–Deschamps ratio of 1.5 (Figure 1).
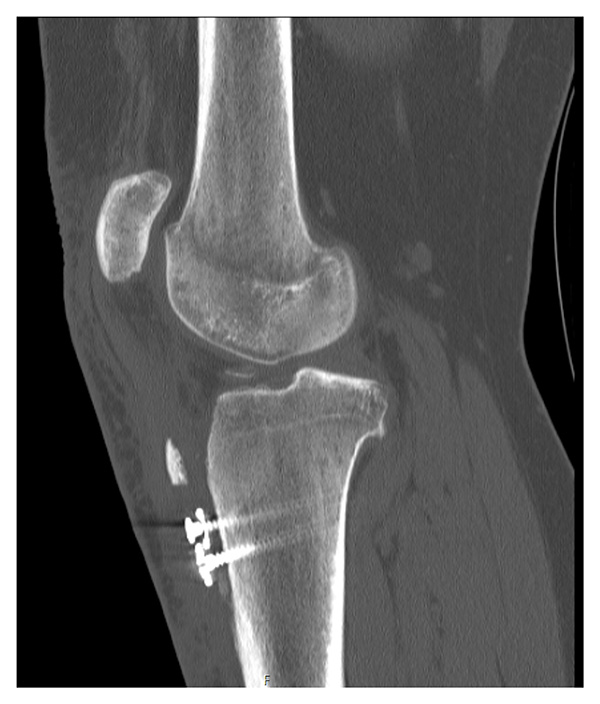
Figure 1: Lateral left knee CT image prior to TTO revision surgery.
To address patella alta and tibial tubercle fracture/nonunion, she was indicated for arthroscopy and revision TTO. Diagnostic arthroscopy noted grade 2–3 fraying on the lateral trochlea and good fill of the previous cartilage restoration to the patella. Both the medial and lateral compartments were intact. Large osteophytes in the notch and a large, inflamed ligamentum mucosum were excised.
An incision was made using the distal aspect of the previous scar. Sharp dissection of the medial and lateral aspects of the prior osteotomy was completed up to the patellar tendon. The patellar tendon was subsequently released from the fat pad; 4 bony fragments were skeletonized, and after removing the existing hardware (2 screws and 2 washers), the tibia was debrided at the prior osteotomy site. Bone morphogenetic protein was inserted beneath the shingle. The shingle was subsequently reduced and stabilized with K-wires. Using fluoroscopy in both extension and 30° of flexion, the patellar height was found to be appropriate. A 2.4-mm and a 2.7-mm plate were contoured, placed over the shingle, and secured with 2 medial and 2 lateral screws, compressing the shingle (Figure 2).

Figure 2: Using a small C-arm, fluoroscopy confirmed position of the patella following shingle fixation.
The medial and lateral aspects of the patellar tendon were secured with 4 Krackow stitches, using #2 Orthocord sutures (DePuy Synthes), which were fixed to 2 4.75-mm Peek SwiveLock anchors (Arthrex) on the medial and lateral tibia, distal to the tubercle. With the knee in 30° of flexion, the arthrotomy was closed with interrupted sutures (size 0 Vicryl and 3.0 Monocryl). A hinged knee brace was locked straight for 6 weeks, and the patient was made non-weightbearing.
At 2 weeks postoperatively, she had reached 30° of flexion with the assistance of a continuous passive motion machine. At 6 weeks postoperatively, she had reached 90° of flexion and showed good medial and lateral translation of the patella. A 6-week X-ray (Figure 3) showed the bony fragment (shingle) to have minimally displaced, so she was placed in a long leg cast. She began taking calcium and vitamin D, and she was started on teriparatide by a metabolic bone specialist. At 3 months, a CT scan showed no evidence of healing, and the patient returned to the operating room for a Hernigou procedure with bone marrow aspirate concentrate done under fluoroscopic guidance.

Figure 3: Lateral X-ray of the left knee at 6 weeks postoperatively after revision TTO demonstrates proximal migration of the shingle.
An MRI 4.5 months after the open reduction and internal fixation revision TTO revealed that the patellar tendon had healed to the tibia, but the bony fragments had not healed. A final X-ray at 1 year postoperatively demonstrated complete healing of the tibial tubercle (Figure 4). The patient had full range of motion, was able to reciprocate stairs, and had returned to lacrosse.

Figure 4: Lateral X-ray at 1-year postoperatively demonstrates healed tibial tubercle.
Discussion
A TTO is a well-established procedure for patellofemoral joint pathologies, including patellofemoral instability and chondromalacia, which can improve patellar maltracking and restore the biomechanical function of the patellofemoral joint [1]. Even though studies have shown TTOs to be effective for treating patellofemoral joint conditions, failures including delayed union and nonunion do occur [2-4], with potentially profound effects on a patient’s quality of life, underscoring the necessity for experienced knee surgeons to treat these patients [5]. There is little in the literature on the outcomes of revision surgery following a TTO, although it is known that nonunion following a TTO is a serious complication that poses unique challenges. Even so, surgeons at HSS have been able to help patients undergoing revision TTO return to sports.
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Orthopedic Surgery, Weill Cornell Medical College
Ava G. Neijna, BA
Research Assistant
Hospital for Special Surgery
References
- Shah AK, Uppstrom TJ, Rizy ME, Gomoll AH, Strickland SM. Incidence of complications after tibial tubercle osteotomy and tibial tubercle osteotomy with distalization. Am J Sports Med. 2024;52(5):1274–1281. doi: 10.1177/03635465241235883.
- Klinge SA, Fulkerson JP. Fifteen-year minimum follow-up of anteromedial tibial tubercle transfer for lateral and/or distal patellofemoral arthrosis. Arthroscopy. 2019;35(7):2146-2151. doi: 10.1016/j.arthro.2019.02.030.
- Liu JN, Wu HH, Garcia GH, et al. Return to sports after tibial tubercle osteotomy for patellofemoral pain and osteoarthritis. Arthroscopy. 2018;34(4):1022–1029. doi: 10.1016/J.ARTHRO.2017.09.021.
- Sherman SL, Erickson BJ, Cvetanovich GL, et al. Tibial tuberosity osteotomy: indications, techniques, and outcomes. Am J Sports Med. 2014;42(8):2006–2017. doi: 10.1177/0363546513507423.
- Brinker MR, Hanus BD, Sen M, O'Connor DP. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am. 2013 ;95(24):2170-6. doi: 10.2106/JBJS.L.00803.

