Nivolumab-Associated Myositis and Myocarditis in an 83-Year-Old Woman
From Grand Rounds from HSS: Management of Complex Cases | Volume 8, Issue 3
Case Report
An 83-year-old woman with nasal cavity melanoma, previously treated with resection and radiation, received two doses of nivolumab, a checkpoint inhibitor (CI), and presented with progressive myalgia and weakness starting a few days after her second infusion.
Her examination was notable for ptosis of the right eye, diffuse tenderness to palpation of her upper arms and thighs, and weakness of her proximal quadriceps and psoas muscles. She required assistance for ambulation and thus was hospitalized. Her bloodwork was notable for creatine kinase (CK) levels above 5000 U/L, transaminase levels in the 300 to 400 U/L range, and a troponin level of 0.99 ng/mL. Electrocardiography (EKG) showed no acute changes, and echocardiography demonstrated a normal ejection fraction and no wall motion abnormalities.
Due to concern for nivolumab-induced myocarditis, she was immediately treated with methylprednisolone 1 g. Laboratory tests shortly thereafter showed a troponin level rising to 1.2 ng/mL; she was started on mycophenolate mofetil 1 g twice daily. Right and left heart catheterization demonstrated non-obstructive coronary artery disease, and biopsies of the right ventricle were taken. The troponin level continued to rise, despite treatment with pulse-dose steroids and mycophenolate. She was then given a single dose of infliximab 5 mg/kg IV, and the troponin level peaked at 1.67 ng/mL. She was transitioned to methylprednisolone 500 mg on hospital day 2 and 250 mg on day 3. Her myalgia and muscle weakness improved. Endomyocardial biopsy revealed a lymphohistiocytic myocarditis with interspersed CD8+ T cells and myocyte necrosis, characteristic of CI-associated myocarditis (Fig. 1). Steroids were titrated down as her troponin level improved, which eventually normalized by hospital day 19 on oral prednisone doses of less than 10 mg daily and continuing mycophenolate.
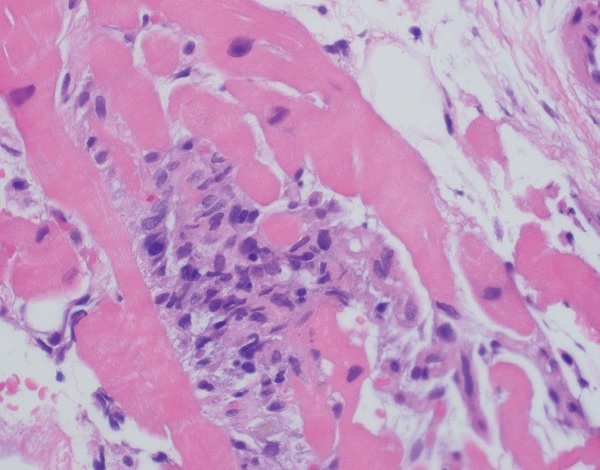
Figure 1: Hematoxylin and eosin staining of right ventricle endomyocardial biopsy showing myocarditis with lymphohistiocytic infiltration.
Discussion
CIs such as nivolumab, a programmed cell death 1 (PD-1) antibody, enhance T-cell-mediated antitumor responses to treat a variety of advanced cancers. However, immune-related adverse events are seen in more than 80% of patients [1] and can affect almost every organ system. Here we discuss a case of CI-associated myocarditis and myositis.
CI-associated myocarditis usually occurs within the first 1 to 2 months of therapy initiation, and the incidence has been suggested to be around 1% [2]. Although it is a rare immune-related adverse event, it carries the highest case fatality rate [3]. Myocarditis often presents with abnormal cardiac muscle enzymes, along with changes in EKG, echocardiography, and/or magnetic resonance imaging, although these radiographic changes are not always present [4]. Characteristic biopsy findings include histiocytic and CD8+ T cell predominant infiltrate [2, 4, 5]. In select postmortem studies of patients who died of CI-induced myocarditis, similar clonal populations of CD8+ T cells were observed in both tumor and cardiac tissue samples, suggesting myocardial injury is due to cross-reactive T cells [5]. Patients with myocarditis may have skeletal muscle involvement, as well. CI-associated myositis can range from asymptomatic CK elevation to rapidly progressive, profound bulbar weakness and respiratory compromise. An accompanying myasthenia-like syndrome with ptosis and bulbar symptoms has also been reported [6].
Treatment of myocarditis and myositis begins with high-dose steroids, although some patients may require other therapies, such as mycophenolate mofetil, intravenous immunoglobulin, or even plasmapheresis [2, 4, 6]. Tumor necrosis factor inhibitors, such as infliximab, are also used, borrowing from their use in the treatment of CI-associated colitis. Myocarditis, if unrecognized, can rapidly lead to life-threatening arrhythmias and/or cardiac failure and should be treated promptly and aggressively. However, the use of multiple immunosuppressive agents can be associated with infectious complications, and steroids should be tapered as soon as possible.
Posted: 10/1/2019
Authors
Attending Physician, Hospital for Special Surgery
Assistant Professor of Medicine, Weill Cornell Medical College
Assistant Attending Physician, Memorial Sloan Kettering Cancer Center
Attending Physician, Hospital for Special Surgery
Professor of Clinical Medicine, Weill Cornell Medical College
References
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373(1):23–34.
- Mahmood SS Fradley MG, Cohen JV, et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71(16):1755–1764.
- Wang DY, Salem JE, Cohen JV, et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and metaanalysis. JAMA Oncol. 2018;4(12):1721–1728.
- Yang S, Asnani A. Cardiotoxicities associated with immune checkpoint inhibitors. Curr Probl Cancer. 2018;42(4):422–432.
- Johnson DB, Balko JM, Compton ML, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375(18):1749–1755.
- Touat M, Maisonobe T, Knauss S, et al. Immune checkpoint inhibitor-related myositis and myocarditis in patients with cancer. Neurology. 2018;91(10):e985–e994.



