Obligatory Patellar Instability in an 8-Year-Old Boy
From Grand Rounds from HSS: Management of Complex Cases | Volume 11, Issue 1
Case Report
An 8-year-old boy presented with recurrent pain and patellar instability of the right knee with increasing difficulty walking and running. Physical examination showed knee range of motion of 0–120° and genu valgum in the right knee worse than the left. Additionally, there was an obligatory lateral dislocation of the patella in knee flexion with spontaneous reduction in extension. The patient had patellar apprehension and was not able to actively extend his right knee from a flexed position. Of note, he had a Beighton score of 4/9, and both his mother and brother had undergone surgery for patellar instability. Radiographs showed mild lateral subluxation of the right patella and a small primary ossific nucleus, consistent with immaturity (Fig. 1).
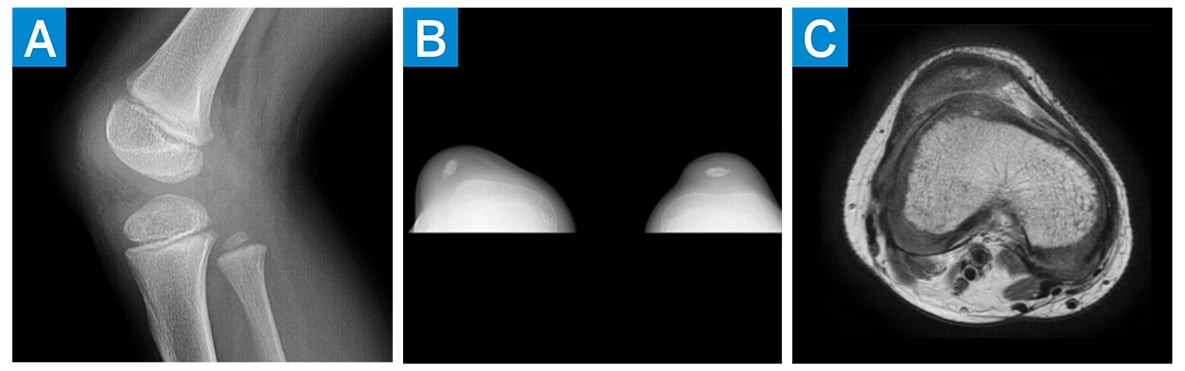
Figure 1: (a) Preoperative lateral X-ray of the patient’s right knee, (b) preoperative merchant view of the knees, and (c) preoperative axial MRI of the right knee.
Magnetic resonance imaging (MRI) demonstrated lateral subluxation of the patella, trochlear dysplasia, and intact articular cartilage (Fig. 1). Surgery was recommended, and the patient underwent the following:
- Right knee medial patellofemoral ligament (MPFL) reconstruction with gracilis allograft to stabilize the patella and prevent future dislocation
- Right knee medial patellotibial ligament (MPTL) reconstruction to enhance stability in flexion
- Right knee medial quadriceps tendonfemoral ligament (MQTFL) reconstruction to add support due to the size of the patella
- Right knee open lateral retinacular lengthening and vastus lateralis tendon lengthening
- Bilateral hemiepiphysiodesis to improve valgus alignment (Fig. 2)
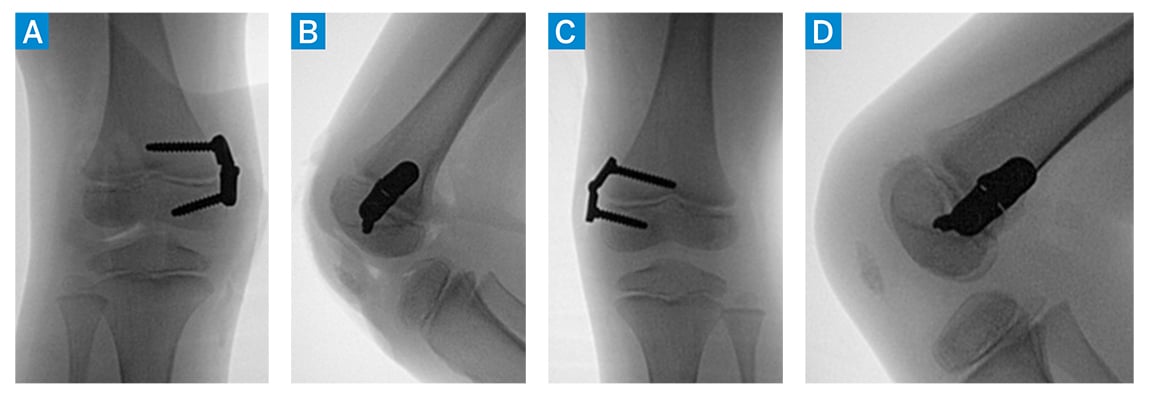
Figure 2: (a, b) Anteroposterior (AP) and lateral intraoperative C-arm images of the right knee after hinge knee plate application. (c, d) AP and lateral intraoperative C-arm images of left knee after hinge knee plate application.
In surgery, a pathologic attachment of the iliotibial band to the patella was noted and released. The patient underwent removal of bilateral hinge knee plates 10 months postoperatively (Fig. 3), at which time he was doing well and reported no pain.
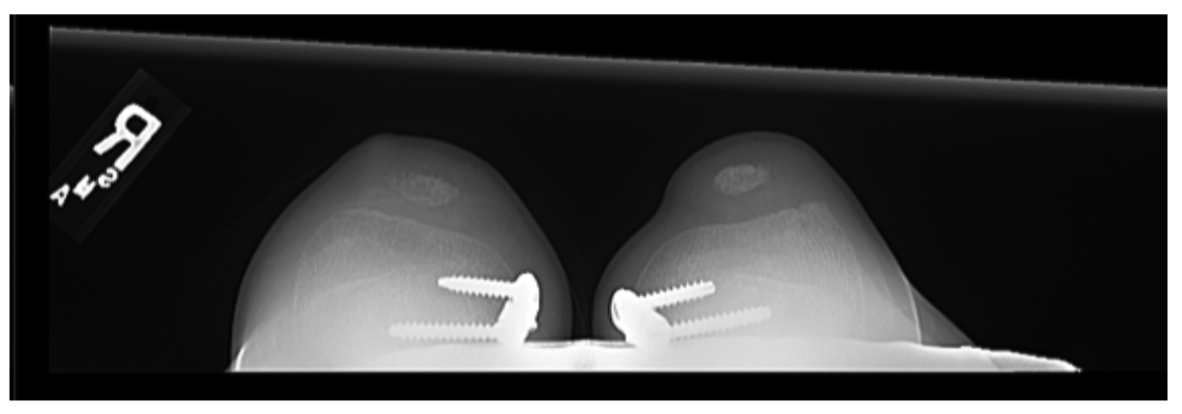
Figure 3: 3 month postoperative merchant view X-ray of the patient’s knees.
Discussion
Patellar instability, represented in about 3% of all knee injuries, occurs most often in people ages 10 to 16 [1]. Genu valgum increases the risk for patellar dislocation and therefore may need to be addressed in skeletally immature patients with patellar instability [2]. Our patient presented with lower limb axis showing valgus alignment, with the mechanical axis alignment off by 15 mm on the right limb and 8 mm on the left limb. Implant-mediated guided growth was used to correct the malalignment. Bilateral plates were left in place for an additional 2 months after achieving correction in order to achieve a desirable amount of overcorrection (Fig. 4) [3]. Such overcorrection decreases the risk of rebound valgus that could lead to future patellar instability.
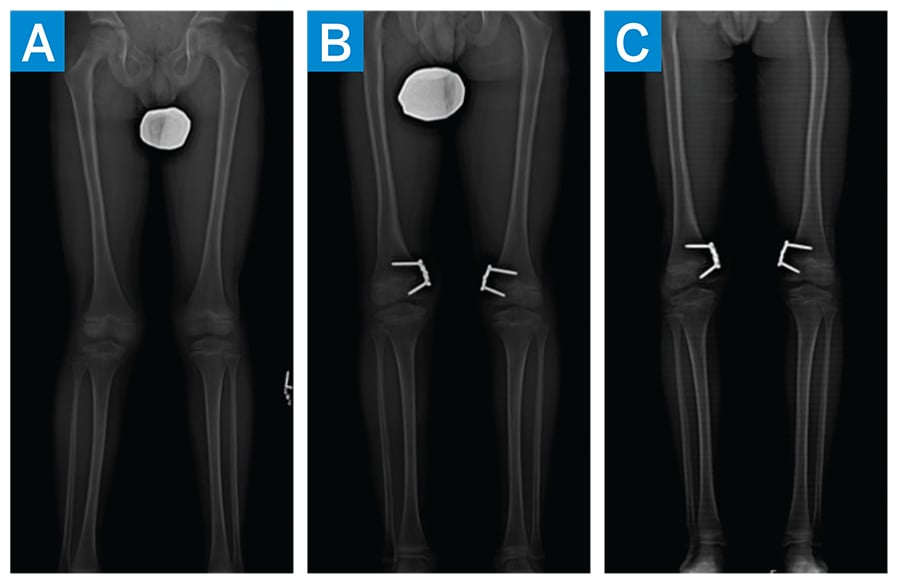
Figure 4: Standing EOS images demonstrating progression of lower extremity alignment. (a) Preoperative (b) 8 months postoperative (c) 10 months postoperative
Patellar instability in skeletally immature patients can be difficult to manage due to the risk for injury of the distal femoral physis. Various operative techniques with the goal of conserving the distal physis have been described [4]. There was concern that this patient had nail-patella syndrome; therefore, given his age and the size of the patella, MQTFL reconstruction was planned. This allowed for graft placement into the quadriceps tendon to provide greater stability than the MPFL reconstruction alone by inserting into the small patella.
Since the patient was presenting with obligatory dislocation in flexion, MPTL reconstruction was also performed in order to provide further stability in flexion. We believe that in cases of obligatory patellar dislocations, the vastus lateralis tendon is more contracted than the other quadriceps tendons, leading to a lateral vector of force on the patella [5]. Due to the obligatory nature of this patient’s instability, lateral release lengthening and vastus lateralis tendon lengthening were performed to lessen both the lateral vector of force and the negative effect of a tight quadriceps mechanism.
This case of an 8-year-old with obligatory patellar dislocation in flexion and concern for nail-patella syndrome demonstrates the various techniques necessary to provide stability to skeletally immature patients with small patellas and improve function.
References
- Koh JL, Stewart C. Patellar instability. Orthop Clin North Am. 2015;46(1):147-157. doi:10.1016/j. ocl.2014.09.011
- Parikh SN, Lykissas MG, Gkiatas I. Predicting risk of recurrent patellar dislocation. Curr Rev Musculoskelet Med. 2018;11(2):253–260. doi:10.1007/s12178-018-9480-5
- Redler LH, Wright ML. Surgical management of patellofemoral instability in the skeletally immature patient. J Am Acad Orthop Surg. 2018;26(19):e405–e415. doi:10.5435/JAAOS-D 17-00255
- Sidharthan S, Wang G, Schlichte LM, Fulkerson JP, Green DW. Medial patellofemoral ligament reconstruction in skeletally immature patients. JBJS Essent Surg Tech. 2020;10(e0110):1–3.doi:10.1097/BTK.0b013e31822ba746
- Ellsworth B, Hidalgo Perea S, Green DW. Stepwise lengthening of the quadriceps extensor mechanism for severe obligatory and fixed patella dislocators. Arthrosc Tech. 2021;10(5):e1327-e1331. doi:10.1016/j. eats.2021.01.034

