Managing High-Energy, Proximal Tibia and Fibula Fracture in a 37-Year-Old After a Skiing Accident
From Grand Rounds from HSS: Management of Complex Cases | Volume 12, Issue 1
Case Report
While skiing at high speed, a 37-year-old man lost control, struck his left lower leg against a tree, and sustained a complex proximal tibia and fibula fracture initially managed with an external fixator. There were no signs of compartment syndrome, and except for Crohn’s disease treated with vedolizumab, he was healthy. He traveled home 3 days after injury on deep vein thrombosis (DVT) prophylaxis with enoxaparin.
At presentation 1 week after injury, the patient was neurovascularly intact with resolving fracture blisters. The external fixator pin sites showed no evidence of infection. Radiographs showed a complex, largely extra-articular, proximal tibia fracture with dissociation of the tibial tubercle (Fig. 1). Subtle findings of a proximal lateral tibia avulsion fracture (a Segond fracture) and tibial spine comminution raised suspicion for ligamentous knee instability. Diastasis of the proximal fibula from the tibia demonstrated the high energy nature of the trauma. A computed tomography (CT) scan showed the complex proximal tibia fracture with a separate tibial tubercle fragment and confirmed a posterior cruciate ligament (PCL) avulsion fracture and lateral proximal tibia avulsion (Fig. 2). Magnetic resonance imaging (MRI) confirmed a lateral meniscal root tear, disruption of the PCL, proximal tibiofibular capsular ligaments, and moderate posterolateral corner injury (Fig. 3).

Figure 1: Anteroposterior (AP) radiograph shows spanning external fixation.

Figure 2: 3D CT reconstruction.
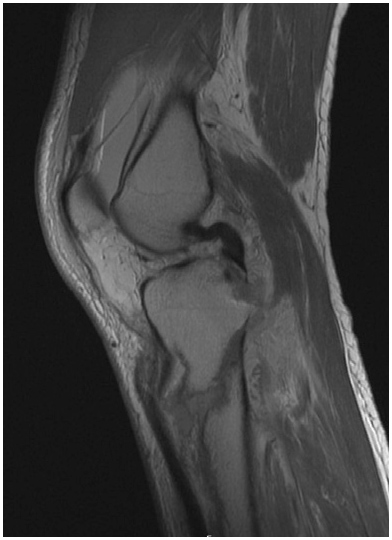
Figure 3: MRI shows a secondary deformity of the PCL due to avulsion of the PCL footprint, with a slightly displaced footprint fracture.
Preoperative planning with orthopaedic trauma and sports medicine teams called for stable bony fixation, capsule and PCL repair, and tibiofibular proximal joint stabilization.
Intraoperative fluoroscopy radiographs showed near anatomic restoration of the bony anatomy (Fig. 4). Multiple minifragment plates and independent lag screws were used for fragment-specific fixation and provisional reduction control. The proximal tibial locking plate was used after fragment-specific fixation in neutralization mode for definitive fixation. The bony PCL avulsion fragment, including the insertion of the posterior horn of the lateral meniscus, was repaired using proximal and distal button fixation bridged with SutureTape. This was accomplished via the posteromedial approach utilized for bony fixation that was extended intracapsularly. An iatrogenic ramp lesion (meniscocapsular separation) was created to improve exposure, and this was repaired primarily upon closure. The fibula was reduced and secured with a screw.
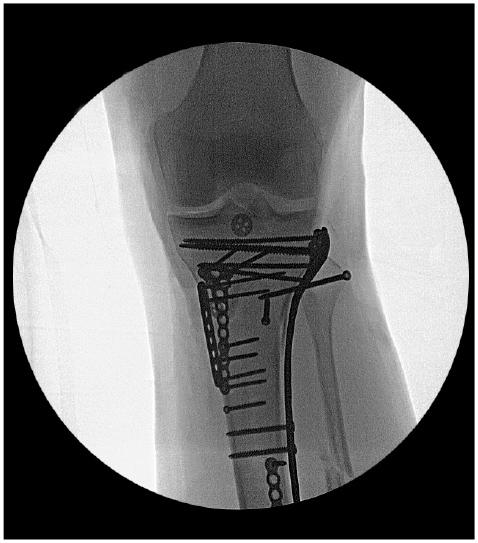
Figure 4: Intraoperative AP fluoroscopic radiograph shows near anatomic reduction.
Radiographs at 6 weeks postoperatively showed the fracture was healing (Fig. 5), and the patient had regained flexion to just beyond 90°. By 3 months, he had regained nearly normal range of motion (Fig. 6), had a stable knee exam, and normal gait.
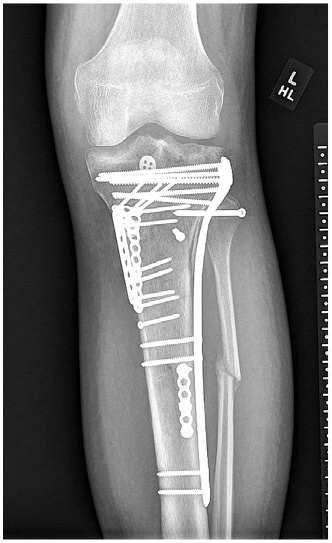
Figure 5: AP radiograph at 6 weeks postoperatively shows maintenance of alignment.

Figure 6: Photograph at 3 months postoperatively shows range of motion and flexion.
After several months of physical therapy, his motion, strength, and endurance were restored. At 18 months postoperatively, the fracture had fully healed and the patient had returned to skiing.
Video: Gregory S. DiFelice, MD, demonstrates the patient’s range of motion 3 months post-surgery.
Discussion
We have found that proximal tibia fractures, especially those involving high energy trauma and Segond fractures [1, 2], are often associated with ligamentous and/or meniscal pathology. The optimal timing of managing both bone and soft-tissue damage remains unclear, but managing both simultaneously, as in this case, can provide bony and ligamentous stability in the knee, allowing for early and aggressive rehabilitation [3]. This case demonstrates several other principles of proximal tibia fracture management:
- Patients with high-energy, proximal tibia fractures are at risk for compartment syndrome [4].
- DVT prophylaxis should be considered in patients with proximal tibia fractures.
- We manage the pin sites by stabilizing the pin–skin interface with a bulky dressing for 5 to 7 days to promote epithelialization, recommending daily showers thereafter [5].
- The principles of spanning external fixation include placing the external fixator pins out of the zone of injury and of future hardware and restoring length and alignment.
- Mini-fragment fixation is commonly used to hold a reduction and to buttress fragments [6].
- Simultaneous fracture and ligament repair can be quite effective with modern day suspensory fixation, potentially avoiding the need for late reconstructions.
References
- Porrino J, Richardson ML, Hovis K, Twaddle B, Gee A. Association of tibial plateau fracture morphology with ligament disruption in the context of multiligament knee injury. Curr Probl Diagn Radiol. 2018;47(6):410-416. doi: 10.1067/j.cpradiol.2017.09.001.
- Peltola EK, Mustonen AO, Lindahl J, Koskinen SK. Segond fracture combined with tibial plateau fracture. Am J Roentgenol. 2011;197(6):W1101-4. doi: 10.2214/AJR.10.6095.
- Ismailidis P, Kernen R, Egloff C, Nüesch C, Mündermann A, Müller SA. Clinical and biomechanical outcomes of one-stage treatment of a simultaneous ipsilateral patellar tendon and ACL tear combined with a tibial plateau fracture: a case study. Case Rep Orthop. 2020;2020:5793948. doi: 10.1155/2020/5793948.
- Marchand LS, Working ZM, Rane AA, Elliott IS, Gilbertson E, Rothberg DL, Higgins TF, Haller JM. Compartment Syndrome in Tibial Plateau Fractures: Do Previously Established Predictors Have External Validity? J Orthop Trauma. 2020 May;34(5):238-243. doi: 10.1097/BOT.0000000000001703. PMID: 31738237.
- Kazmers NH, Fragomen AT, Rozbruch SR. Prevention of pin site infection in external fixation: a review of the literature. Strategies Trauma Limb Reconstr. 2016;11(2):75-85. doi: 10.1007/s11751-016-0256-4.
- Chen MJ, Frey CS, Salazar BP, Gardner MJ, Bishop JA. Low profile fragment specific plate fixation of lateral tibial plateau fractures - A technical note. Injury. 2021;52(4):1089-1094. doi: 10.1016/j.injury.2020.12.037.


