Recurrent Periprosthetic Joint Infection Treated With Total Femur Spacer and Subsequent Acetabular Component Conversion
From Grand Rounds from HSS: Management of Complex Cases | Volume 13, Issue 1
Case Report
A 69-year-old man presented with an infected left revision hip replacement. He had undergone total hip arthroplasty (THA) in the 1980s for avascular necrosis, was later revised for aseptic loosening in 2003, and then developed systemic signs of sepsis following a chronic toe wound. He was treated with a 2-stage revision with placement of an antibiotic spacer and eventual reimplantation with a modular tapered stem. The reimplantation was complicated by a periprosthetic fracture requiring fixation; infection recurred within 2 months. The patient underwent 2 subsequent irrigation and debridement procedures and was on oral doxycycline and fluconazole for infection suppression when presenting to HSS.
Assessment found a 4-in. leg length discrepancy, limited hip flexion to 60°, and pain and an audible clunk. Radiographs showed a revision construct with a multi-hole acetabular component fixed with multiple screws and a modular tapered stem with cerclage wires that had subsided (Fig. 1). Notably evident was a proximal femur fracture, joint dislocation, and an aggressive periosteal reaction along the diaphysis and distal metaphysis of the femur, which raised concerns for underlying osteomyelitis. With regular monitoring, antibiotic and antifungal therapies were stopped for 2 weeks, and hip aspiration was positive for Corynebacterium and Candida albicans. Due to the polymicrobial culture results and involvement of most of the femur, an explant of the revision hip replacement, resection of the distal femur, and insertion of a total femoral replacement spacer were planned.
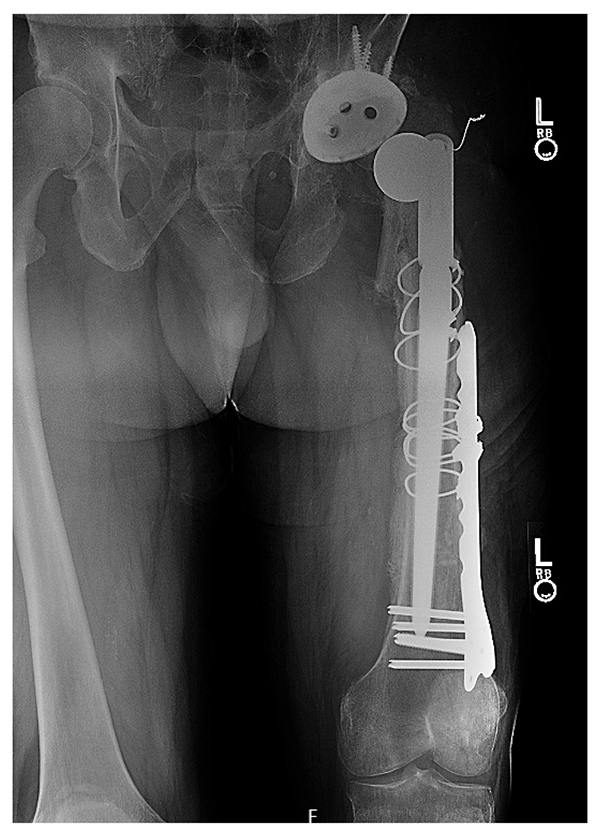
Figure 1: Preoperative X-ray shows a revision arthroplasty construct most notably with catastrophic subsidence of the femoral component and evident periosteal reaction along the distal femur.
An extensile posterolateral approach and separate midline approach to the left knee were performed with 2 surgical teams simultaneously. All components were safely removed, the proximal tibia was cut, and the patella was debrided. A distal femoral component (Stryker GMRS) was implanted and coated with high viscosity cement (Palacos R+G) containing gentamicin 0.5 g, vancomycin 2 g, and voriconazole 400 mg per bag (Fig. 2). To maximize hip stability due to posterior-wall bone loss, a 64-mm bipolar head was used (Fig. 3). Deep surgical drains were placed, and negative pressure dressings were applied to the incisions.

Figure 2: Intraoperative photo shows a total femoral component coated with polymethylmethacrylate cement containing antibiotics and antifungals.
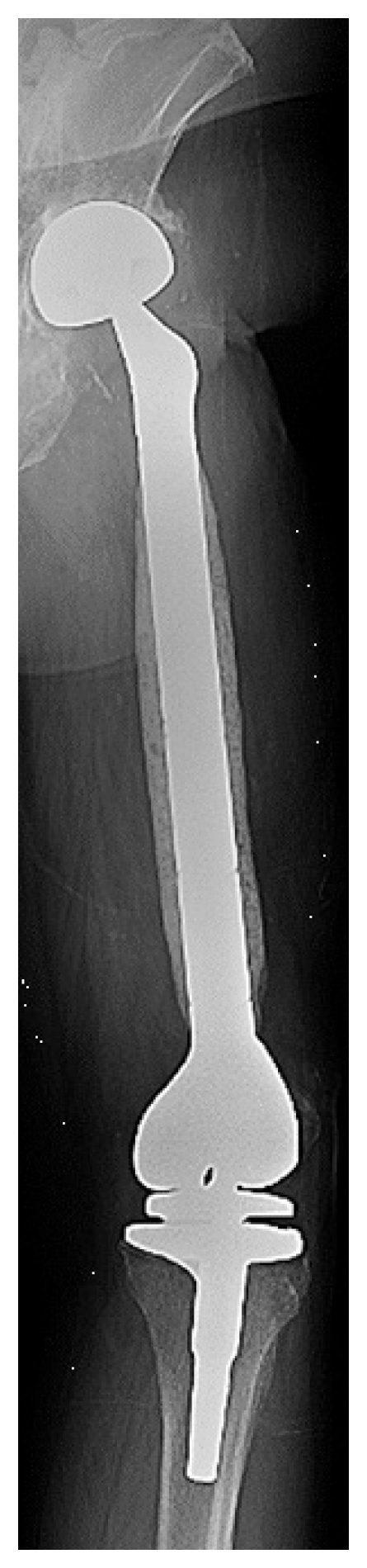
Figure 3: Postoperative radiograph demonstrates the total femoral component spacer and large bipolar head articulating with the acetabulum.
Postoperatively, the leg length discrepancy had improved, with the external shoe lift decreased from 4 in. to 1.5 in. The patient was hospitalized for 2 weeks for treatment with IV vancomycin, piperacillin, and caspofungin; after 6 weeks he transitioned to oral doxycycline and fluconazole. After 4 months, he began weight bearing with crutches, but at 6 months he noticed persistent groin pain. Radiographs (not shown) raised concerns for possible acetabular erosion secondary to the bipolar head. He was placed on a 2-month antimicrobial holiday, with blood and aspiration samples indicating no infection.
The patient underwent robotic-assisted conversion from a bipolar hemiarthroplasty to THA involving a revision acetabular component (Stryker Trident 2) (Fig. 4). Robotic assistance was deemed necessary due to posterior and medial wall bone loss. Intraoperative cultures were negative. Postoperative pain was substantially reduced, and he was discharged home after 5 days. At 6 weeks postoperatively he sustained a posterior dislocation that was reduced in an emergency room. At 1-year follow-up, the patient used a crutch to mobilize, had a ¾-in. shoe lift, perceived no leg length discrepancy, and was off antibiotics and antifungals.
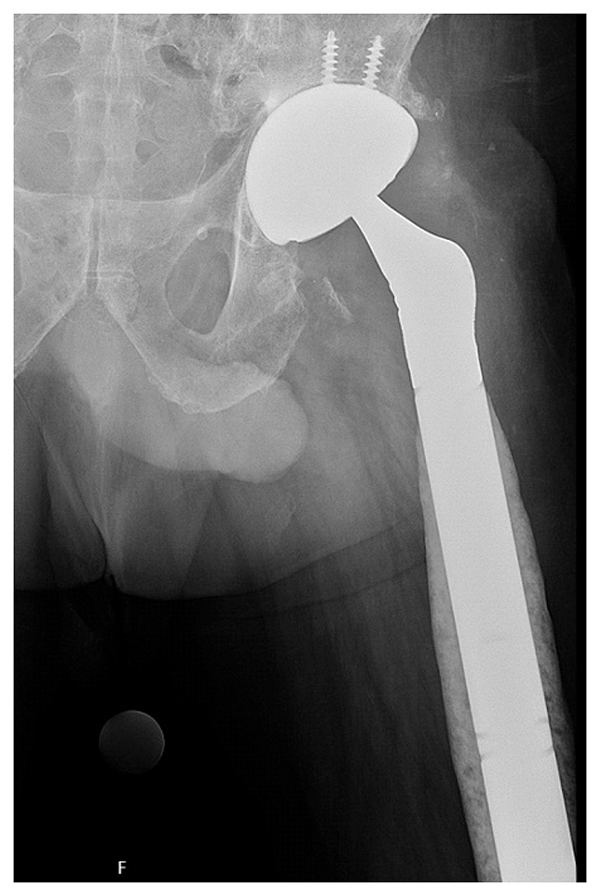
Figure 4: Postoperative radiograph demonstrates the revision acetabular component with secondary screw fixation following robotic-assisted conversion.
Discussion
A 2-stage revision for chronic periprosthetic joint infection (PJI) has a roughly 80% success rate, but recurring infection substantially decreases the chance of success [1,2]. Furthermore, the presence of polymicrobial [3] and fungal [4] infection is a negative prognostic indicator. The use of a total femoral antibiotic spacer is a technically demanding limb-salvage treatment for complex PJI that involves compromise of over half the femur. This radical procedure is associated with reasonable success in preventing infection recurrence in up to 75% of cases [5], but patients often require ambulatory assistive devices and careful monitoring due to risk of complications [6], including postoperative instability and mechanical loosening of the knee component. Our experience in using 2 surgical teams substantially shortens procedure duration, reducing both blood loss and anesthesia time.
This case also highlights the utility of robotic assistance in acetabular revision, although it is not typically feasible due to artifacts on imaging from the acetabular component. However, bipolar hemiarthroplasty makes computed tomography-based bony segmentation possible, so that the robotic arm can be safely oriented.
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor, Weill Cornell Medical College
Attending Orthopedic Surgeon, Hospital for Special Surgery
Assistant Professor of Orthopedic Surgery, Weill Cornell Medical College
Chief Emeritus, Surgical Arthritis Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery
References
- Simon S, Frank BJH, Gardete S, et al. Analysis of failed two-stage procedures with resection arthroplasty as the first stage in periprosthetic hip joint infections. J Clin Med. 2021;10(21):5180.
- Shichman I, Ward SA, Lu L, et al. Failed 2-stage revision knee arthroplasty for periprosthetic joint infection-patient characteristics and outcomes. J Arthroplasty. 2023;38(10):2177-2182.
- Marculescu CE, Cantey JR. Polymicrobial prosthetic joint infections: risk factors and outcome. Clin Orthop Relat Res. 2008;466(6):1397-1404.
- Koutserimpas C, Naoum S, Alpantaki K, et al. Fungal Prosthetic joint infection in revised knee arthroplasty: an orthopaedic surgeon’s nightmare. Diagnostics (Basel). 2022;12(7):1606.
- Heidenreich MJ, Tetreault MW, Lewallen DG, Perry KI, Hanssen AD, Abdel MP. Total femur antibiotic spacers: effective salvage for complex periprosthetic joint infections. J Arthroplasty. 2021;36(7):2567-2574.
- Theil C, Moellenbeck B, Puetzler J, Klingebiel S, Schwarze J, Gosheger G. Two-stage exchange using a total femur spacer in the management of periprosthetic joint infection—spacer complications and implant survivorships. J Arthroplasty. 2023;38(10):2171-2176.




