DEXA Bone Density Tests: A Patient's Guide
Osteoporosis has been called a "silent" disease because the loss of bone progresses gradually without pain or symptoms until a fracture occurs. The best test to determine the state of your bones is called a DEXA scan, also known as a bone density test.
What is a bone density test?
A bone density test is a low-level X-ray measuring important bone sites. The most commonly performed bone density test is called a DXA test (sometimes written as “DEXA”). DXA stands for Dual-energy X-ray Absorptiometry. (DXA is the term preferred by the ISCD – the International Society for Clinical Densitometry. However, “DEXA” is more widely used and recognized by people outside the medical profession.)
Schedule a DEXA scan at HSS. (A prescription is required.)
Low-level X-rays, equivalent to less than two day’s exposure to natural background radiation, measure important bone sites (detailed below). It is painless, non-invasive, and takes about 10 minutes.
Who should have a DEXA bone density test?
Anyone who meets the following criteria should get a DXA test.
- women 65 years of age or older
- men aged 70 and older
- adults with a fragility fracture (fracture with little or no trauma, such as a fall from standing height)
- adults with a disease or condition associated with low bone mass or bone loss
- adults taking medications associated with low bone mass or bone loss
- adults with lifestyle factors that lead to bone loss, such as smoking and excessive alcohol intake
- women during the menopausal transition and men younger than 70 with risk factors for low bone mass including low body weight and prior fracture
- women who have lost more than 1.5 inches and men who have lost more than two inches from their tallest height
What happens during a DEXA scan?
You will be asked to stop taking calcium supplements 24 to 48 hours before the scheduled DXA exam (different facilities have different guidelines). Metal jewelry (for example, belly button piercings) and clothing with metal fasteners (zippers, buckles, hooks) should be avoided.
Fully clothed, you will lie flat on your back on a padded table. Legs may be straight or positioned on a padded platform. A scanner will pass over your lower spine and hip while another scanner passes beneath you. At HSS, the wrist is scanned with the same machine while you are seated next to the machine. Other facilities may use a separate scanner to evaluate the wrist.
You may be asked to hold your breath during the scanning, ensuring that you lie very still so that motion artifact does not interfere with the images the technologist and radiologist evaluate on the computer screen.
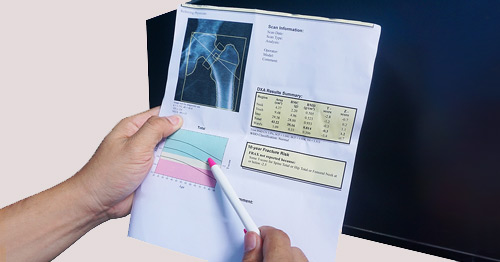
What do my DEXA scan bone density test results mean?
DXA bone mineral density for different sites on the skeleton is reported as grams per centimeter squared (gm2) – measuring the amount of calcium and other bone materials packed in to a segment of bone. Values are compared to others of the same age and gender (Z-scores) or healthy young adults at peak bone mass (T-scores).
For post-menopausal women and men age 50 and over, the result of DXA is based on T-scores:
- A T-score equal to or above -1.0 is considered normal bone density.
- A T-score between -1.0 and -2.5 is considered low bone density, sometimes referred to as osteopenia.
- A T-score -2.5 or below is considered osteoporosis.
The World Health Organization (WHO) established the following skeletal sites for diagnosis: the lumbar spine, the total hip, the femoral neck (a part of the hip in the upper portion of the femur bone) and, in certain circumstances, the 33% radius (the wrist).
Osteoporosis anywhere in your body is osteoporosis everywhere. The diagnosis is made using the lowest T-score. For example, if the T-score in your spine is -2.7 and the T-score in your hip is -2.2, the diagnosis is osteoporosis. It is incorrect to say there is osteoporosis in the spine and osteopenia in the hip.
For people with low bone density, the FRAX (fracture risk assessment) tool, is often included in the report. Using femoral neck bone density (the bone density of a portion of the femur) and patient-specific data, the 10-year probability of a major osteoporotic fracture and a hip fracture is generated.
Your results may also include a TBS – trabecular bone score. This reflects the microarchitecture of bone in the spine. Results are classified as normal, partially-degraded, and degraded.
Depending on your clinical circumstances and risk factures, your healthcare provider may also include a vertebral fracture assessment (VFA) for the spine and/or a femur fracture assessment (FFA) for the hip.
Does arthritis show up on a bone density test?
Osteoarthritis – degenerative joint disease − is unrelated to osteoporosis (this is a common point of confusion). Osteoarthritis in the spine and hip may increase measured bone mineral density. If degenerative disease is present, your healthcare provider will focus on unaffected regions of interest. The trabecular bone score is not impacted by osteoarthritis.
At what age should you stop getting bone density tests?
Unlike various cancer screening modalities, there is no upper age limit for bone density screening.
Updated: 8/10/2022
Authors
Physician, Ambulatory Care Center, Hospital for Special Surgery
Clinical Assistant Professor of Medicine, Weill Cornell Medicine