Advanced Technology in Hip and Knee Replacement Surgery at HSS
The range of technologies used in total hip and knee replacement surgeries has changed tremendously since surgeons at HSS pioneered the first modern artificial knee replacements in the 1970s.

While HSS offers the latest cutting-edge techniques, we recognize that no technology is a substitute for a skilled and experienced surgeon. Our surgeons use an innovative, evidence-based approach to develop the best surgical plan for each individual patient.
A number of technologies have changed the way that joint replacement surgeries are done. These include robotics and computer navigation, 3D printed implants, smart sensors and other wearables and augmented reality. HSS is at the leading edge of adapting these technologies, using them to provide the best care for all our patients.
Arthroscopic or minimally invasive surgery, which uses small instruments and incisions that are less than an inch long, is available for certain orthopedic procedures. But because knee replacement surgery requires surgeons to remove and replace a substantial portion of bone, knee replacement surgery cannot be done in what is traditionally been considered an arthroscopic or minimally invasive approach.
Robotic joint replacement
Robotic surgical arms allow surgeons to maximize the precision and individualization of hip and knee replacement surgery. The robotic arm helps the surgeon ensure that each step of their surgical plan is precisely executed as intended.
Prior to surgery, tracking devices called arrays are placed around the patient’s knee or hip. These devices communicate the location, position and orientation of the hip or knee to the robotic arm. If the position changes, the robotic arm can make real-time alignment adjustments or halt the procedure until the surgical team repositions the patient accordingly.
During the operation, both the surgeon and the robotic arm hold the surgical tools. The arm prevents these tools from deviating outside the alignment of the surgeon’s plan. At the same time, during the operation, if the surgical team identifies that minor adjustments to the plan are necessary, they can make these and recalibrate the computer.
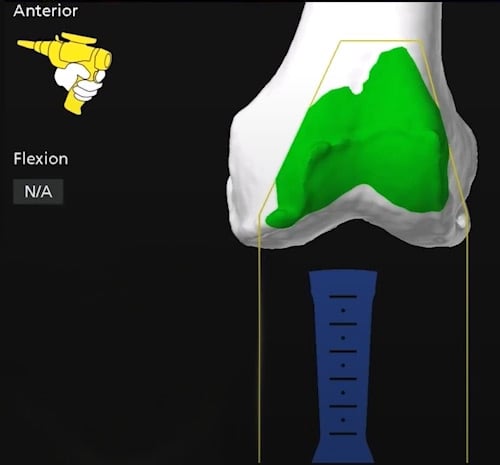
Computer navigation image of a robotic arm used by an orthopedic surgeon on the front of the femur, prior to osteotomy.
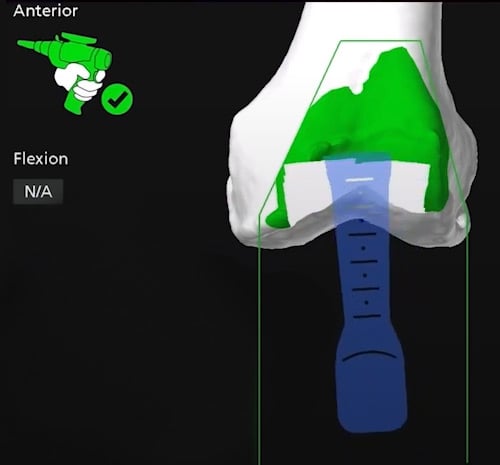
Computer navigation image of the robotic arm at the start of the osteotomy to remove bone from the front of the femur.
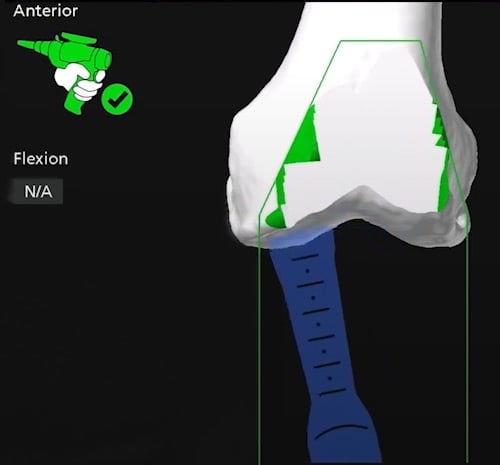
Computer navigation image of the robotic arm near completion of the knee osteotomy to prepare the femur for an implant.
After the prosthetic implants are in place, the computer can capture 3D renderings of the postsurgical alignment of the new joint and the position of the implants. These real-time 3D images allow the surgeons to assess the stability and alignment of the knee and make any necessary adjustments before the surgery is complete. (Learn more about robotic knee replacement.)
Computer navigation
Computer navigation involves the use of special software and sensors to create a 3D model of a patient’s knee or hip joint prior to surgery. The surgeon can then use this model during the joint replacement procedure to aid in place of the implant.
In knee replacement surgery, specifically, computer navigation can help the surgeon to align the new knee joint with the patient’s bones and ligaments. Achieving alignment is important because it can increase the overall stability of the joint and reduce the risk of instability and other complications.

In hip replacement, the surgeon may use computer navigation to help position the hip socket. Proper positioning is critical to the function of the new joint.
It is important to note that this technology is not suitable for every patient or for every type of joint replacement. However, there is evidence to show that computer navigation in hip and knee replacement surgery generally can result in more precise surgeries, in turn this may lead to less pain and better function for the patient.
Advanced imaging
Imaging techniques such as X-ray and MRI have always been important before, during and after hip and knee replacement surgery. One new technique now proving beneficial is 3D motion capture technology. This technology uses an array of cameras to track a patient’s motion in real time to provide enhanced views of the joint for surgical preplanning and during the procedure itself.
After surgery, HSS surgeons may use a technique called fluoroscopy to analyze the biomechanical performance of a patient’s knee implant and assess how closely it mimics the natural movement of the knee. Fluoroscopy is a kind of imaging that uses a continuous high-resolution X-ray. It allows the doctor to view internal images of the body in real time and to assess the joints and their motions from almost any angle.
This technique allows surgeons to not only assess healing but also to uncover other critical elements of a patient’s recovery, including how the soft tissues and ligament structures are affecting movement.
Augmented reality technology
In early 2021, HSS performed the first augmented reality-assisted knee replacement in the United States. In this variation of computer navigation, surgeons wear augmented reality (AR) “smart glasses,” which allow them to visualize the structures of the patient’s knee and track surgical progress in real time by superimposing the images above the surgical field. With this technique, the surgeon doesn’t have to turn their head to look over at a computer screen. This technology has the potential to improve implant positioning.
3D printing technology
The ultimate goal for any joint replacement is to design an implant that will function for the rest of a patient’s life. For some patients, 3D-printing technologies allow HSS surgeons to construct joint implants tailored to their specific anatomy. These customized implants may reduce or eliminate the need for fixatives like bone cement.
Customized implants also offer enhanced ability of the natural bone to grow into the implant. This is particularly important for patients with more complex conditions, including those who have previously had other implants fail.
In 2021, HSS and LimaCorporate opened the first hospital-based 3D design and printing center. This facility enables HSS to create customized orthopedic implants for certain patients who require complex joint reconstruction surgery.
"Smart" implants and wearable technology
Wearable technologies and “smart” implants are transforming surgical recovery. They are also enabling more active partnerships between the patient, surgeon and physical therapist.
In October 2021, HSS surgeons performed the first-ever knee replacement that incorporated a prosthetic implant with a smart sensor. The sensor has the ability to measure a patient’s steps, walking speed, range of motion and other indicators of knee function following surgery. The technology used is similar to that found in many cardiac pacemakers, which is used to collect data that’s sent to a patient’s cardiologist.
Once implanted, the smart knee records and wirelessly transmits data that allows surgeons to check on a patient’s progress, especially for the first year after their surgery. The data collected by the implant is sent to a device that plugs into an outlet at the patient’s home. It is then securely sent to a cloud-based platform, where the healthcare team can review it to check on the patient’s progress and recovery and make adjustments to their physical therapy regimen if necessary.
Smart implants and devices such as smart rings and watches allow doctors and physical therapists to track patients’ activities. Wearable sensors help physical therapists assess the impact of certain movements on a patient’s leg after knee replacement surgery.
All of these technologies allow providers to measure the quality of a patient’s recovery and to intervene early and suggest modifications if there is an issue.
Pain-reducing techniques
Joint replacement surgery at HSS is usually done with spinal anesthesia (commonly known as an epidural) rather than general anesthesia. Because this type of anesthesia wears off gradually, it helps control pain immediately after surgery.
Additionally, when the spinal anesthesia wears off, patients may be offered nerve blocks in the area around the joint replacement. Medicines injected into the nerves above the knee can provide 24 to 36 hours of pain relief.
These technologies, combined with medications including anti-inflammatories, nerve pain medications and antidepressants, help to reduce the need for narcotics and facilitate a speedy recovery.
Data collection and research advances
From the time a patient at HSS receives their first X-ray or MRI, data is being collected. This data – whether gathered via imaging, gait simulation or physical therapy – allows surgeons to better understand the patient’s anatomy as well as to study the outcomes of different surgical approaches.
No other orthopedic institution has the volume of patient data that HSS does. Our collaborative joint replacement registry includes data on more than 55,000 patients. Every one of our hip and knee replacement surgeons participates in ongoing clinical research, using the data collected to help assess new technologies. This research helps us to guide the development of new standards in joint replacement surgery, impacting patients today and in the future.
Reviewed and edited by the Adult Reconstruction and Joint Replacement Service
References
- Pagan CA, Karasavvidis T, Cohen-Rosenblum AR, Hannon CP, Lombardi AV Jr, Vigdorchik JM. Technology in Total Knee Arthroplasty in 2023. J Arthroplasty. 2024 Sep;39(9S2):S54-S59. doi: 10.1016/j.arth.2024.07.028. Epub 2024 Jul 23. PMID: 39053667. https://pubmed.ncbi.nlm.nih.gov/39053667/
