Minimally Invasive Lower Back Surgery for Disc Degeneration: The Anterolateral (Side) Approach
A minimally invasive surgical approach to lumbar spine fusion
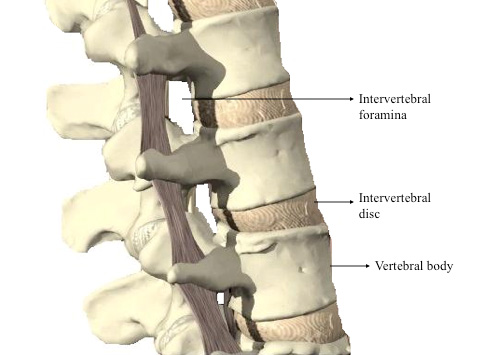
The spine consists of 33 bones called vertebrae that provide body structure and protect the spinal cord (Figure 1). Linking the vertebrae are intervertebral discs and facet joints that absorb shock and allow for movement and flexibility. As people age, the discs between vertebrae lose water, decreasing the ability of the discs to cushion the spine. This process is called disc degeneration and can reduce the space through which nerves exit, called the intervertebral foramen.
Figure 1: Anatomy of the spine. 3D anatomy images copyright of Primal Pictures Ltd.
Spinal fusion
Spinal fusion is a surgical treatment option for conditions such as degenerative disc disease. The objective of the procedure is to stabilize and immobilize the joint between two vertebrae, which will alleviate pain and improve back function. In an interbody fusion, the damaged intervertebral disc is replaced with a specially designed cage that maintains proper alignment of the spine and restores proper disc height. Interbody fusions can be performed in the cervical or thoracic sections of the spine (neck and upper back, respectively), but they are most commonly performed in the lower back. These are known as lumbar interbody fusions.
Realigning the spine and restoring disc height enlarges the space through which nerves exit. Furthermore, these cages contain harvested bone and growth factors that will stimulate the vertebrae to grow together, or fuse. A growth factor called bone morphogenetic protein, or BMP, is commonly packed into these cages to encourage bone growth.
Traditional approached for lumbar interbody fusion
There are several traditional approaches to access the spine for an interbody fusion. Generally, these are either a posterior (from the back) approach or anterior (from the front or chest) approach.
- A posterior approach provides direct access to the spine but involves disrupting major back muscles and manipulating nerves that can lead to pain and loss of sensation after the surgery. Learn more in Posterior Lumbar Interbody Fusion (PLIF).
- A traditional anterior approach provides excellent access to the spine, and from this approach surgeons can restore collapsed disc spaces, release and correct spinal deformities such as scoliosis, and ultimately help patients achieve solid fusions. Accessing the front of the spine through a traditional anterior approach spares the back muscles and nerves but involves large incisions and requires careful manipulation of the major blood vessels and organs of the abdomen. Learn more in ALIF Surgery: Anterior Lumbar Interbody Fusion.
Lateral lumbar interbody fusion (LLIF)
A more recently developed lateral approach (from the side), known as a lateral lumbar interbody fusion, may also be used and offers several advantages over the traditional approaches while maintaining the benefits of an anterior exposure of the spine. In this minimally invasive technique, the patient is positioned on his or her side (Figure 2).

Figure 2: Patient positioned for the lateral lumbar interbody fusion.
The surgeon will identify the affected disc using X-ray and mark the appropriate position for a small, lateral incision. Through this incision, the psoas muscle is the only muscle that will need to be transversed (Figure 3).
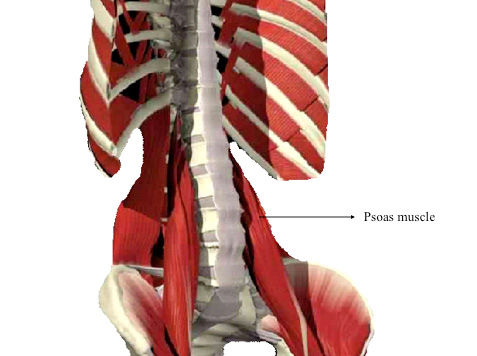
Figure 3: The psoas muscle lies against the lower spine. This is the main muscle transversed (crossed) in the lateral approach to the spine. Once transversed, the disc space is exposed laterally (on the side of the disc). 3D anatomy images copyright of Primal Pictures Ltd.
Neurologic monitoring devices are used to dissect through the psoas muscle, lowering the risk of nerve injury. Once the disc space is exposed, the surgeon meticulously releases the deforming forces of the spine and prepares the bones for fusion. The damaged disc is removed and the specialized cage is implanted.
These far lateral techniques to access the spine may be combined with posterior approaches to obtain complete reconstruction of the spine. Alternatively, the anterior approach from a far lateral technique may be done as a stand-alone procedure for certain patients.
Benefits and complications of the lateral interbody fusion
Benefits
One benefit of the lateral approach is that incisions made in this position can be significantly smaller than incisions of the traditional approaches. In addition, approaching the spine from a lateral incision avoids many of the vital organs, muscles, and vessels that may be disrupted by the traditional approaches, decreasing the likelihood of post-operative abdominal muscle weakness and hernias.
As a result, patients who undergo surgery using this far lateral approach to the lumbar spine commonly experience less blood loss and tissue trauma, improved mobilization, and faster recovery times.
Possible complications
As a result of disruption of the psoas muscle and the nerves around it, some patients may experience thigh and/or groin pain or numbness. Usually, these symptoms are temporary and resolve within a few months after the surgery.
In choosing the best approach, the surgeon will consider the patient’s anatomy and condition as well as the benefits and risks of each technique. Patients should discuss with their doctor which technique is right for them.
Oblique lumbar interbody fusion (OLIF)
More recently, a truly anterolateral approach (meaning from the side but also slightly from the front of the patient) has been developed to avoid disrupting the psoas muscle. It is most appropriate for patients in whom nerve damage is of particular concern and/or for the lowest vertebrae (L4-L5 and sometimes L5-S1), which are difficult to access using the direct lateral and far lateral approaches. The OLIF approach is at roughly a 45-degree angle to the patient’s abdomen, versus the roughly 90-degree angle in the direct lateral approach and the slightly posterior far lateral approach.
Authors
HSS Spine
Hospital for Special Surgery