Tibial Spine Fractures in Children: What to Know
What is a tibial spine fracture?
A tibial spine fracture (also known as an avulsion fracture) is a type of injury that commonly occurs in children between the ages of 8 and 14. It happens when the anterior cruciate ligament (ACL) pulls a small piece of bone away from the tibia. This injury usually occurs during low-velocity sports or a fall, where the knee is twisted or hyperextended.
What are the types of tibial spine fracture?
In the past, doctors used a system called Myers McKeever (MM) to classify these fractures. Tibial spine fractures were classically categorized into three basic grades, with the third being the most severe:
- Grade I is a non-displaced fracture, where the tibial spine remains in position.
- Grade II is a partially, anteriorly displaced fracture, where a front portion of the tibial spine is detached but a posterior (rear) portion remains intact.
- Grade III is a completely displaced fracture, where the tibial spine is fully separated from the tibia.
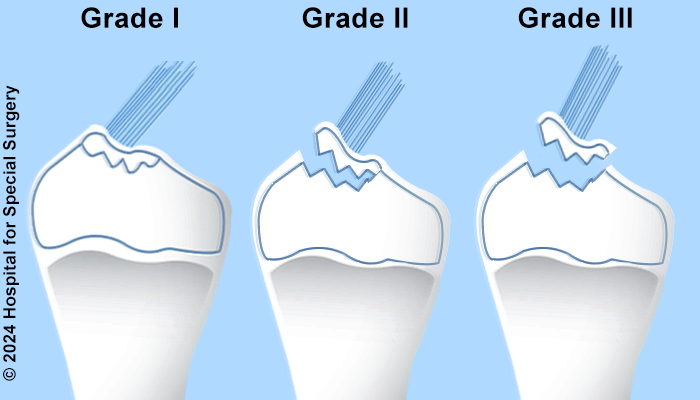
Illustration of the Myers and McKeever classification system
How is a tibial spine fracture diagnosed?
Diagnosing and treating tibial spine fractures using X-rays alone used to be complicated and controversial. But now, doctors have better tools like magnetic resonance imaging (MRI) that can show more details about the fracture and any other injuries that may have occurred with it. In fact, about 60% of children with tibial spine fractures also have other injuries like meniscal tears.
The Myers McKeever (MM) classification system was based on looking at simple X-rays, which cannot show soft tissue damage. But now, researchers at HSS have developed a new way to classify tibial spine fractures using MRI. It looks at things like the size and pattern of the fracture, how much the bone has moved, and if there are any entrapments (when soft tissue gets stuck in between the bones). This new system is based on numbers and measurements instead of just looking at pictures.
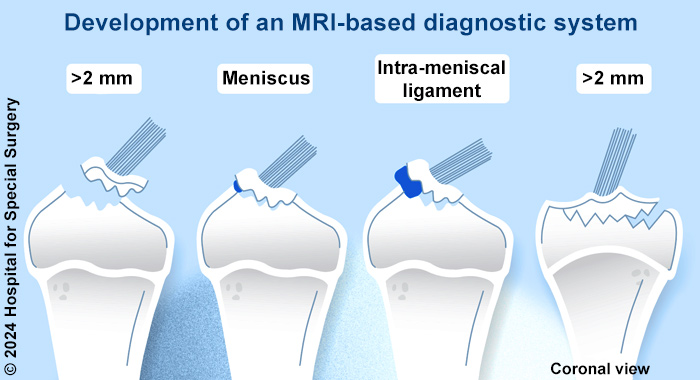
Illustration of tibial spine fractures variables measured using a new MRI-based diagnostic system, such as a bony displacement of greater than two millimeters, involvement of the meniscus, or entrapment of soft tissue in the fracture gap (such as the intra-meniscal ligament, as shown).
“Determining which patients with tibial spine fractures need to have surgery has been problematic with the standard classification system,” says HSS pediatric knee surgeon Daniel W. Green, MD, MS, FAAP, FACS, who developed the new system with HSS pediatric orthopedic research colleagues and HSS radiologist Gabrielle P. Konin, MD. “But surgery is important in reducing the risk of scar tissue, which affects 10% to 20% of kids with this injury.”
When can surgery be a benefit?
The new way of classifying tibial spine fractures developed at HSS has changed the treatment recommendations for about one-third of patients. This means that some patients who may have been told they needed surgery before may not need it under the new system, and some patients who would have been told they didn't need surgery before may actually benefit from it.
At HSS, doctors use this new classification system to help decide on the best treatment for each patient. It also helps them identify any concomitant injuries (other injuries that happen at the same time) that may need to be treated.
HSS radiologists have also developed special MRI protocols for children with tibial spine fractures. These protocols give doctors even more detailed information to help make the best treatment decisions.
HSS research on treatments for tibial spine fractures
HSS is part of a research group that focuses on improving outcomes for patients with tibial spine fractures. They work with other top hospitals to study the best ways to classify and treat these injuries.
One important finding from their research is that MRI identified additional injuries in 45% of patients with tibial spine fractures, which can greatly affect treatment decisions. This is why MRI is now recommended for all children with tibial spine fractures.
Another important discovery is that 23% of patients developed a condition called arthrofibrosis after surgery. This is when the knee joint becomes stiff and difficult to move. To help prevent this, it is important for children with tibial spine fractures to have stable surgical fixation (when the bones are put back together) and start moving their knee soon after surgery.
If a child does develop arthrofibrosis, they may need to return to the operating room to improve motion.
“We hope our findings help more surgeons become aware of arthrofibrosis risk in patients with tibial spine fractures so that patients may receive specialized care when appropriate,” says Dr. Green.
Posted: 2/23/2024
Authors
Chief of the Pediatric Orthopedic Surgery Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery
Attending Radiologist, Hospital for Special Surgery
Associate Professor of Radiology and Imaging, Weill Cornell Medical College
Related articles
References
- Cruz AI Jr, Lee RJ, Kushare I, Baghdadi S, Green DW, Ganley TJ, Ellis HB Jr; PRiSM; Tibial Spine Research Interest Group; Mistovich RJ. Tibial Spine Fractures in Young Athletes. Clin Sports Med. 2022 Oct;41(4):653-670. doi: 10.1016/j.csm.2022.05.006. PMID: 36210164.
- Green D, Tuca M, Luderowski E, Gausden E, Goodbody C, Konin G. A new, MRI-based classification system for tibial spine fractures changes clinical treatment recommendations when compared to Myers and Mckeever. Knee Surg Sports Traumatol Arthrosc. 2019 Jan;27(1):86-92. doi: 10.1007/s00167-018-5039-7. Epub 2018 Jun 30. PMID: 29961096.
- Salvato D, Green DW, Accadbled F, Tuca M. Tibial spine fractures: State of the art. J ISAKOS. 2023 Dec;8(6):404-411. doi: 10.1016/j.jisako.2023.06.001. Epub 2023 Jun 13. PMID: 37321295.




