
![]()
The HSS Global Musculoskeletal Health Equity Division (GMHED) is a humanitarian group based within Hospital for Special Surgery that is dedicated to empowering our partners in resource-limited settings to build and lead essential training programs and care centers in the musculoskeletal health field.
Poor access to safe and effective surgical and anesthesia care is a problem that dominates the current global health landscape. Musculoskeletal disease occupies a large proportion of this problem. More than five billion people worldwide, most of whom reside in resource-poor areas, lack access to limb and life-saving surgery and anesthesia. Reduced musculoskeletal health care capacity, especially provider shortages, means injuries, deformities and degenerative conditions often go untreated. When treatment is available, it is commonly provided at understaffed hospitals, which is correlated with high complication rates and suboptimal pain management.
In the 21st century, there are increasing calls to action by international health authorities to address these inequities. While providers historically travelled to resource-limited settings to care for patients directly, we now know that supporting locally led education and research is more cost-effective and sustainable.
Learn more about our program, staff and initiatives in the tabs below.

In 2012, Swetha Pakala, MD founded the Global Health Initiative (GHI) within the Department of Anesthesiology, Critical Care & Pain Management. The focus of this program was to address the need for improved anesthetic capacity in low-resource settings by supporting regional anesthesia training. GHI’s first program was conducted at the Hospital for Traumatology and Orthopedics in Ho Chi Minh City, Vietnam. The program later expanded its work to sites in Uganda, Ghana and India.
In 2017, GHI launched GRACE (Global Regional Anesthesia Curricular Engagement), which was a novel training model for resource-limited settings. GRACE enabled us to create teaching curricula using a systematic framework based on a partner site’s specific needs. It also offered a platform with which to measure intervention outcomes. Learn more about GRACE
Due to the success of our anesthesia programs and the need for greater musculoskeletal surgical capacity in RLS, HSS endorsed the creation of GMHED in 2021. The HSS Global Musculoskeletal Health Equity Division is a division of HSS Global Partnerships founded by Swetha Pakala and Mark Brouillette to provide humanitarian services in places where the need for musculoskeletal care is great and access to safe high-quality care is lacking.
The program aims to incorporate all of the relevant service lines under the HSS musculoskeletal health care umbrella. A multidisciplinary program like this has the potential to increase the positive impact on providers and patients in resource-limited settings.
The GMHED mission is to improve musculoskeletal education, research and practice at our partner institutions in resource-limited settings at home and abroad by supporting clinical training programs, building local research infrastructure, and supporting efficient quality improvement innovations.
Our vision and guiding principles are to develop and deploy evidence-based, adaptable methods to assess the musculoskeletal health care needs of hospitals in low-resource settings and evaluate the impact of global health initiatives aimed to address gaps in training, research and care while observing the following principles:
Using Implementation Science to guide a systematic and outcomes-based approach to global health, we are utilizing the RE-AIM framework. Starting with a stakeholder meeting with all relevant members, each service line conducts a needs assessment to understand the needs of their specialty at a RLS site. The result of a needs assessment is a specifically tailored intervention that is meant to improve capacity. In our experience with both of our currently active sites, we have found that the need for subspecialty training in many areas is without a doubt, the overwhelming need.
After instituting the intervention with our team and local champions, we then evaluate the intervention using RE-AIM. Our goal is to teach until we find the local providers are self-sufficient and can then perpetuate the learning to their colleagues and trainees.
Below is a graphic representation of our GHMED model:
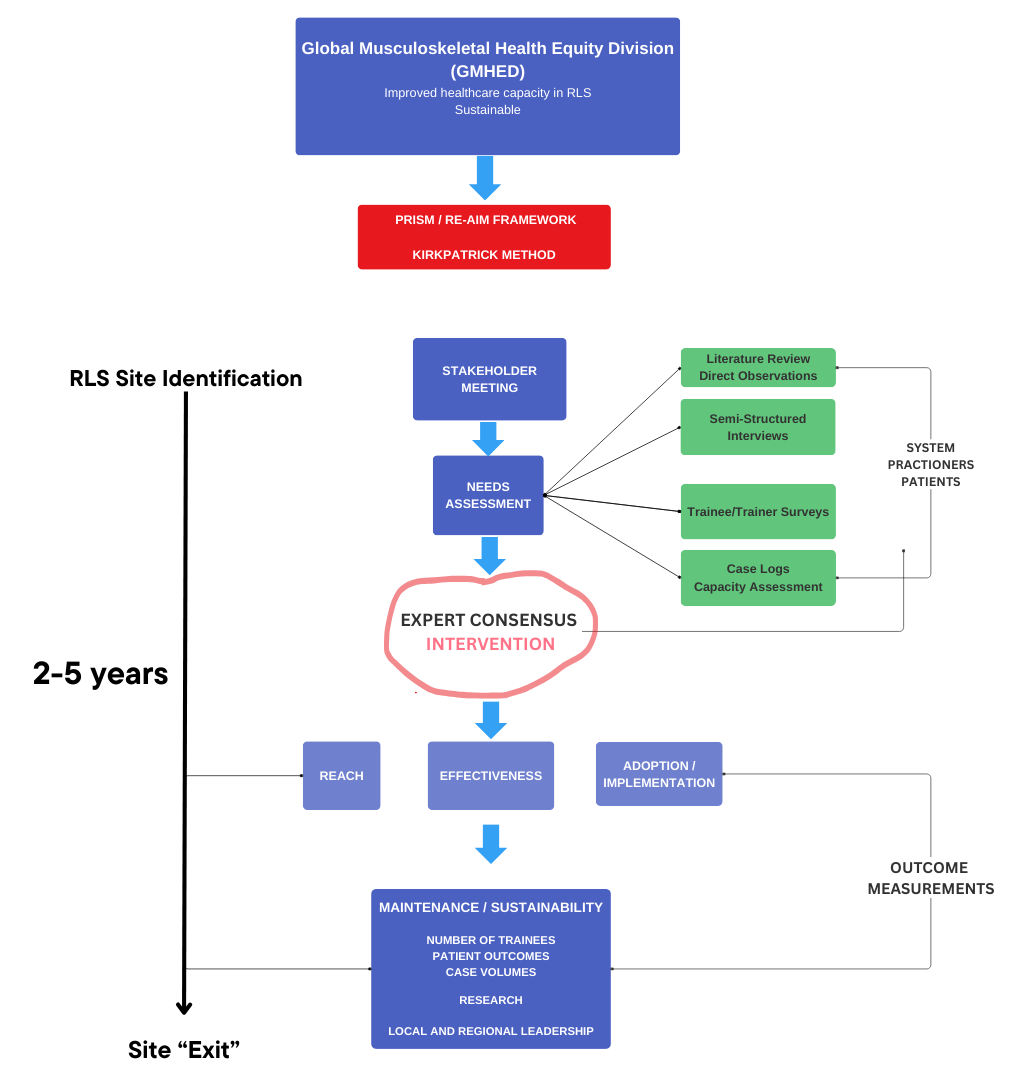
Each of our sites, and each service line at these sites, are in different stages of this model. Ultimately, our goal is to exit a site after 2-5 years, once we have confirmed self-sufficiency among the local providers. While we provide continuing education and feedback, it is mostly limited to virtual exchanges with the RLS.

Swetha Pakala, MD
Co-Chair GMHED

Mark Brouillette, MD
Co-Chair GMHED

Jawad N. Saleh, B.S., Pharm.D., BCPS, BCCCP
Executive Director

Andrew Grose, MD, MSc
Orthopedic Surgery

Mark Brouillette, MD
Anesthesia

Swetha Pakala, MD
Anesthesia

Harmandeep Singh, MD
Chronic Pain Management

Niharika Thakkar, PhD
Research

Adelin Bharat
Alfred Aidoo, MD
GMHED Site Director, Ghana

Madhavi Julakanti, MD
Professor of Anesthesia
GMHED is currently active at two sites in RLS: Ghana and India.
Each site is in different stages of progress within the GMHED framework.
The Republic of Ghana has a population of 31 million and is situated along the Gulf of Guinea in West Africa. Ghana is a multinational state that gained independence from the British in 1957. The government is a unitary constitutional democracy, and English has been adopted as the common language. With respect to musculoskeletal disease, the burden of trauma, chronic degenerative states and congenital deformities is high, but much of the infrastructure and workforce needed to care for these conditions is lacking. GMHED currently collaborates with the two largest teaching hospitals in Ghana. Our programs there focus on increasing the orthopedic surgery and anesthesiology workforce by training local doctors and conducting research.
Komfo Anokye Teaching Hospital (KATH): Kumasi, Ghana
HSS and KATH began working together in 2017, though Dr. Brouillette has led several US academic centers’ global health programs with the KATH Directorate of Trauma and Orthopaedics and Directorate of Anaesthesia & Intensive Care. KATH is a 1,200-bed academic center built in 1952 and located in the city of Kumasi. KATH is the primary referral center for the northern two-thirds of Ghana and the teaching institution for the Kwame Nkrumah University of Science and Technology Medical School. More than 10,000 surgeries are performed at KATH annually; 16% for musculoskeletal conditions, many of which are road traffic injuries. KATH offers postgraduate medical training in most disciplines, including Trauma & Orthopaedics and Anaesthesia & Intensive Care.
Dr. Harman Singh is currently leading the pain management global health initiative to establish and validate a framework for improving chronic pain care access through partnerships, education, training and capacity building in resource-limited settings. Currently, he is collaborating with Komfo Anokye Teaching Hospital (KATH) in Ghana to help establish a chronic pain division, train new pain management fellows, increase chronic pain management capacity, and improve access to care for patients.
Dr. Jawad Saleh is leading GMHED’s pharmacy branch. He has focused on areas such as global pharmacy assessments and standardization efforts to significantly improve healthcare outcomes in under-resourced regions, ensuring equitable access to quality pharmaceutical services and contributing to overall health system strengthening.
Based on our unique needs assessment, including input from the government to the local interests of nurses and surgeons we idenitified the need for subspecialty fellowships in all fields of orthopaedics (they currently have only generalists) with the plan to make Komfo Anokye Teaching Hospital a center of orthopaedic excellence. This involves partnerships with Harvard and University of Calgary, for domains like musculoskeletal oncology and sports medicine, as well as internal partnership with Foundation for Orthopaedics and Complex Spine for planned spine and arthroplasty fellowships.
This year we started with our trauma program, using an OTA-based curriculum developed in concert with the Ghanaian College of Physicians and Surgeons. Dr. Andrew Grose is supervising this, with visiting experts from Netherlands (Diederik Verbeek & Peter Kloen), Canada (Geoffrey Wilkin & Allan Liew), and the US (David Wellman, Gele Moloney, Jaimo Ahn, Milan Sen, Kanu Okike, Jason Mckean and Charles Cornell).
With respect to the orthopaedic aspect of our work in Ghana, this project includes training of nursing, surgical techs, central sterile professionals, and will also include upgrades to anesthesia machines, OR tables, and hopefully new central sterilization systems. We have also worked to find cost-effective but good quality instrument/implant supply to make this sustainable within the Ghana economy.
India, officially called the Republic of India, is the seventh largest country by area, the second most populous country and the largest democracy in the world. It is a pluralistic, multilingual, and multi-ethnic society. India has become a fast-growing major economy and a global hub for information technology services. Despite the economic advances, India is also overwhelmed by unyielding poverty, both urban and rural. Additionally, religious and caste-related prejudice permeates many sectors of society. In poverty-plagued communities, healthcare resources and workforce are dire, which leads to a high burden of disease. Musculoskeletal disease, particularly trauma, comprises a large proportion of unmet need.
Osmania General Hospital (OGH): Hyderabad, India
HSS and OGH began working together in 2019 when the HSS anesthesia Global Health Initiative (GHI) introduced the GRACE training model to the OGH department of anesthesiology. OGH is the second largest government hospital in South India and provides free medical care to the indigent population of Hyderabad and the surrounding areas. OGH houses 1,000 beds within three specialty buildings, has 62 operating rooms of various specialties and performs roughly 62,000 surgeries per year. OGH offers the premier anesthesiology residency training program in South India, with approximately 90 new residents annually. Although physician anesthesiologists have been performing regional anesthesia techniques for several years, there is a large variability in skill and success rates among practitioners. The OGH faculty therefore sought to collaborate with GHI to improve their knowledge and skill level.
Initiated the GRACE Training Protocol to teach ultrasound-guide regional anesthesia to a group of 14 members of the OGH Anesthesia Department.
Point-of-care ultrasound (POCUS) has become quite popular in the U.S. because of its wide range of uses and benefits. However, in the field of anesthesiology, there is a lack of standard practice and training, especially in low-resource settings. Additionally, the utility of POCUS is tremendous in RLS, as the modality enables immediate diagnosis and intervention without the need for prohibitively expensive imaging. We conducted an assessment at Osmania General Hospital (OGH) to understand the specific training needs for POCUS. This helped us create a tailored training program that fits the needs of these settings and ensures it is sustainable.The GMHED team organized a week-long, hands-on training course for POCUS in February of 2023, which included fellows, experienced anesthesiologists, and POCUS experts. We collected and analyzed data before and after the training to measure its effectiveness. We returned to OGH for a follow-up refresher course in December 2023. Our experience in India helped us develop a blueprint for POCUS training that can be used in other low-resource settings.
We are currently in the needs assessment phase for trauma at OGH. Dr. Jason Mckean teaches orthopedic trauma at OGH while assessing their needs.
In 2013, Dr. Swetha Pakala launched a global health track of the HSS Regional Anesthesiology & Acute Pain Medicine Fellowship. One to two fellows per year have the opportunity to take part in the Global Health Track. Dr. Brouillette and Dr. Pakala serve as the fellow’s mentors and help them gain an in-depth understanding of existing global musculoskeletal health care disparities as well as the traditional versus modern strategies used to address health care inequities. Fellows will also have the chance to design and execute an academic project at one of our GMHED sites or at a low-resource institution of their choosing at home or abroad, travel safety guidelines permitting. This is typically a concise education or research-focused project that can be completed and disseminated in the fellowship year. Up to four weeks of travel is sponsored depending on the project specifications.
Fellows will graduate from our track with an enhanced appreciation for the unmet orthopedic needs worldwide, evidence-based tools to join or build new global health initiatives in their future careers, and enhanced fluency in multidisciplinary and cross-cultural communication and collaboration. Based on the project of each fellow’s choosing, he or she will have the opportunity to teach the expertise they have learned at HSS in a low-resource setting. To date, completed teaching programs have included ultrasound-guided regional anesthesia and point of care ultrasound (POCUS).
2013/2014: Carolyn Dejean and Jesse Ng
2014/2015: Anjali Rosario
2015/2016: Lee Rasamny
2016/2017: Lauren Nakazawa
2017/2018: Mark Brouillette and Patrick Loughlin
2018/2019: Benjamin Johnson and Joseph Keaveney
2020/2021: Kareem Zuaiter and Mark Harris
2021/2022: Desean Thom
2022/2023: Erica Tafuro and Lucia Lee
2023/2024: Monica Anise and Jason Haidar
The Global Musculoskeletal Health and Equity Division at the Hospital for Special Surgery is dedicated to advancing global health equity through cutting-edge research and innovative approaches. Our research approach is grounded in Implementation Science and the RE-AIM model, ensuring that our findings are not only scientifically robust but also practically applicable and impactful on a global scale.
Implementation Science is a key focus of our research strategy. This discipline emphasizes the systematic uptake of research findings and other evidence-based practices into routine practice, thereby improving the quality and effectiveness of health services and care. By leveraging Implementation Science, we aim to bridge the gap between research and practice, ensuring that our discoveries lead to real-world health improvements.
The RE-AIM model further guides our research efforts. RE-AIM stands for Reach, Effectiveness, Adoption, Implementation, and Maintenance, and it provides a comprehensive framework for evaluating the impact of health interventions. This model helps us to:
By integrating Implementation Science and the RE-AIM model, our division ensures that our research is not only innovative and evidence-based but also practical and sustainable. This approach allows us to make significant strides in improving musculoskeletal health and equity worldwide, ultimately enhancing the quality of life for individuals and communities across the globe.
GMHED is committed to mentoring interns or research assistants who are interested in global health within the musculoskeletal space.
Current interns:
Johnson and Johnson
Synthes
Americares
Project cure
FOCOS Orthopedic Hospital
UCSF: University of California, San Francisco: Center for Health Equity in Surgery and Anesthesia
Harvard Musculoskeletal Oncology
Texas Children's Hospital
University of Calgary Sports Medicine
WFSA: World Federation Society of Anesthesiologists
ASRA: American Society of Regional Anesthesia
USABCD: UltrasoundAirwayBreathingCirculationDolor
GMHED is currently funded through the generous support of HSS, and operates with the assistance of implant/equipment donations from Synthes and Johnson & Johnson. We are actively working to fundraise for the program, in order to expand the scope of our work.
If you are interested in donating to this important cause, please visit www.hss.edu/give and enter GMHED as the designee for the donation.
Thank you!!
To get in touch with the GMHED team, please contact the Anesthesia Office at 212.606.1206.