Lupus Nephritis Program
Lupus nephritis (kidney involvement in lupus) is a relatively common - and perhaps the most important - complication of systemic lupus erythematosus (SLE), with potentially serious consequences for the patient’s health. Early recognition and effective management is therefore crucial for optimal outcomes.
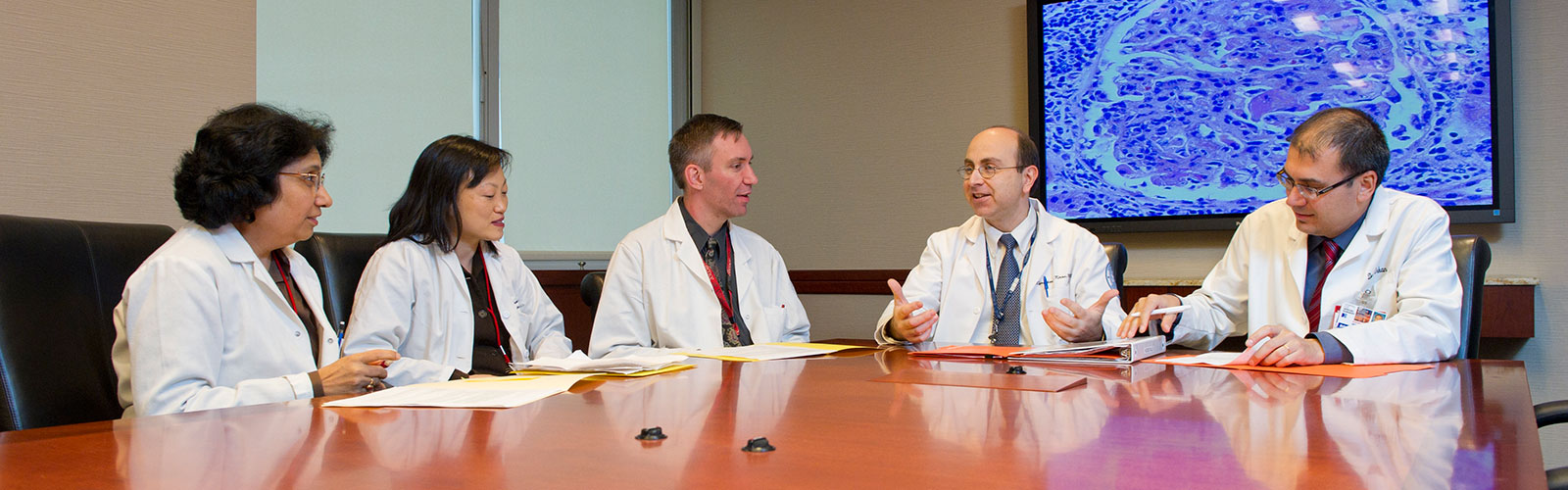
Our goal at the Lupus and APS Center of Excellence is to provide the best possible care for our lupus nephritis patients by using the exceptional resources available to us at Hospital for Special Surgery, NewYork-Presbyterian Hospital, and Weill Cornell Medicine. In order to achieve this goal, we have established the Lupus Nephritis Program under the leadership of Kyriakos Kirou, MD, Clinical Co-Director of the Mary Kirkland Center for Lupus Research. Our approach to treating lupus nephritis is multidisciplinary and includes close collaboration of our rheumatologists, nephrologists, kidney pathologist, nurse practitioner, and infusion room nurses.
As part of the MKCLC monthly Friday conferences, we hold regular multidisciplinary conferences on lupus nephritis where we discuss challenging cases, their optimal therapy, and outcomes.
About Lupus Nephritis
Lupus nephritis is the disease of the kidneys due to lupus. About 30% of lupus patients will develop kidney disease within the first six months to three years of their diagnosis with SLE. In patients with lupus nephritis, an excessively active immune system attacks the patient’s organs and tissues and causes inflammation and damage. Inflammation of the kidney prevents it from functioning normally and can result in the spill of protein and blood in the patient’s urine. As a result, the urine may appear bloody, frothy, or foamy. Other early signs of lupus nephritis may include an increase in blood pressure and swelling of the feet, ankles, and the face, specifically around the eyes.
Prompt diagnosis of lupus nephritis and proper classification of the disease allows for selection of the best therapeutic options for each case. A kidney biopsy is often needed to help with such assessment. The final decision as to which therapeutic option is the best for each patient is made by the patient and the patient’s treating rheumatologist and nephrologist after careful discussion of available options.
The goal of the therapy is to fully control inflammation (Induction Therapy) or to achieve at least major improvement in parameters of kidney function (e.g., reduce the amounts of protein lost in the urine, promote improvement in blood level of creatinine) with minimization of symptoms. This is required to prevent further kidney damage and kidney failure. Once good control of the disease is achieved, Maintenance Therapy is used to prevent further flares.
For a more detailed discussion of lupus nephritis and its management, please see our article on Lupus and Kidney Disease.
If you would like access to treatment for Lupus Nephritis, please visit our Lupus and APS Center of Excellence.