Chronic Pelvic Pain Following Childbirth
Case Example
A 32-year-old female presented to Dr. David L. Helfet at the HSS Orthopedic Trauma Service, 3 days after natural vaginal delivery (of her second child) at an outside hospital. Delivery of her first child was uncomplicated. The second pregnancy and delivery were also uncomplicated. She received peripartum, epidural anesthesia for pain control and delivery was not prolonged (approximately 60-90 minutes). The newborn was healthy and large (10 lbs, 22.5 inches). Thirty minutes following delivery the patient experienced sudden onset of severe pain over her pubic symphysis and lower back with pain radiating down the left leg. She did not suffer additional injuries involving the abdominal or urogenital organs or nerve roots and conservative treatment was initiated with a pelvic binder, bed rest and analgesia. She was limited to transfers from bed to wheelchair and indicated a subjective pain rating of 10 out of 10. She was unable to tolerate mobilization or partial weight bearing with crutches or walker. She was referred to the Dr. Helfet for definitive care for pelvic injury and associated pain symptoms following childbirth.
Diagnostic work-up included standard radiographs of the pelvis demonstrating widening of the symphysis pubis of 9 cm and opening of both sacroiliac (SI) joints posteriorly. A CT scan using 2 mm thin cut technique was performed to evaluate the posterior pelvic ring and SI joints. The CT scan demonstrated bilateral sacroiliac joint disruptions. In addition, a MRI scan documented disruption of the pelvic floor and extensive hematoma. Imaging studies revealed an unstable pelvic dislocation with significant symphyseal widening and disruption of the posterior pelvis equivalent to an APC III, or Tile Type C pelvic injury. Open reduction and internal fixation (ORIF) of the pubic symphysis was performed with placement of a contoured 5-hole 3.5 mm pelvic reconstruction plate and screws. Anatomic reduction and stabilization of SI joints were performed using bilateral posterior ilio-sacral screw arthrodesis. Under fluoroscopic control bilateral single 7.3 mm cannulated screws were inserted percutaneously into the body of S1. The perioperative course was unremarkable. She followed up at regular intervals and reported progressive resolution of pain symptoms. The SI screws were removed at 2 years due to mild radiographic evidence of screw loosening. She returned at 2.5 months following hardware removal and reported complete pelvic pain relief and return to pre-injury activities.
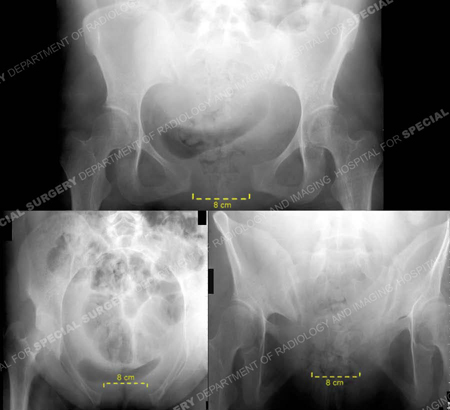
Pelvic views 3 days following vaginal delivery. Anteroposterior, inlet, and outlet views (counter-clockwise) demonstrate separation of the symphysis pubis. The symphysis is separated 9.5 cm and the sacroiliac joints are widened. The left SI joint demonstrates displacement of 9 mm, and the right 8 mm in width. No fractures are identified.
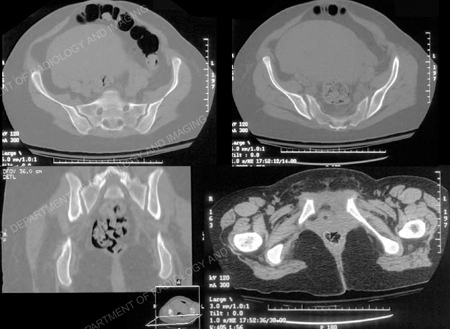
CT examination of the pelvis was performed 3 mm contiguous axial sections. Additional sagittal and coronal reformatted images were also obtained (shown in part). CT findings include symphysis diastasis of 9.5 cm and widening of both SI joints. The left SI joint demonstrates widening of 9 mm, the right SI joint 8 mm with posterior subluxation indicating disruption of the entire right sacroiliac joint. A hairline fracture is noted arising from the right pubic symphysis.

Immediate post-operative radiographic anteroposterior x-ray demonstrating an anatomic reduction of symphysis pubis and symphysiodesis using anterior plating. SI joint reduction and arthrodesis using 7.3 mm cannulated screws have been performed bilaterally.
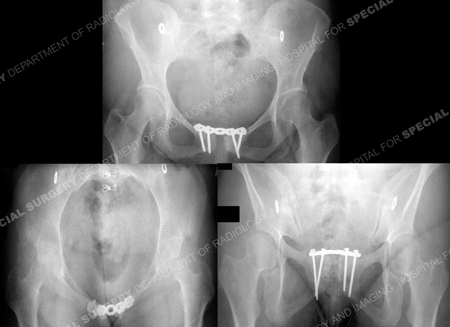
The patient returned at 25.5 months following initial surgery (and 2.5 months following hardware removal) with excellent clinical and radiographic results including a return to pre-injury physical activity.
Research Publications
The HSS Orthopedic Trauma Service has conducted many studies. Please see our publications on sacroiliac joint dislocations.
