About Dr. Bostrom
Dr. Mathias Bostrom is Associate Surgeon-in-Chief and Director of Quality and Safety at Hospital for Special Surgery. He specializes in hip and knee surgery, especially in complex reconstructions and the treatment of musculoskeletal infections. He enjoys the challenges, intellectual and physical, of difficult and complex cases. He is expert in merging old and new technologies, including alternative bearings for younger patients: ceramic, metal, and plastic, where they are appropriate.
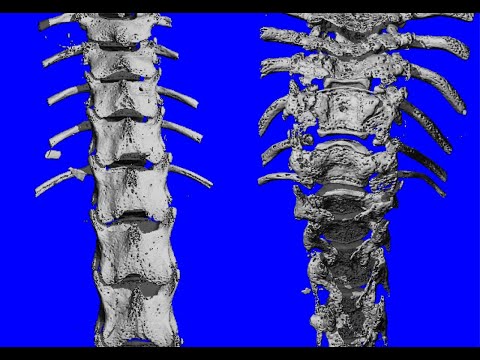
Dr. Bostrom is particularly sensitive to the quality of bone healing and strength. His research focuses on enhancing bone formation, bone regeneration, bone and cartilage healing, and bone biology. He is the author of over 170 journal articles and 22 book chapters. He is a member of numerous prestigious academic orthopedic societies such as the Hip Society, Knee Society, and Orthopaedic Research Society. In addition, he serves as a member of several review panels, including the Musculoskeletal tissue engineering study section of the National Institute of Health.
Dr. Bostrom received his education and training at the University of Virginia and Johns Hopkins. After completing his residency and two fellowships at Hospital for Special Surgery and New York Hospital – Cornell Medical Center, he started his orthopedic practice at Hospital for Special Surgery in 1996.
Profile Video
Special Expertise
Total knee and hip replacement
Hip and knee revisions
Musculoskeletal infections
Videos


Patient ratings for Dr. Bostrom
Insurance
If your insurance is not listed, please call our office if you have questions regarding your insurance coverage. If you have out-of-network benefits, then your insurance may reimburse you for a portion of your office visit.
Credentials
Appointments
Associate Surgeon-in-Chief and Director of Quality and Safety, Hospital for Special Surgery
Chief Emeritus of Adult Reconstruction and Joint Replacement Service, Hospital for Special Surgery
Chief Emeritus of Hip Service, Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery
Professor of Orthopedic Surgery, Weill Cornell Medical College
Attending Orthopedic Surgeon, NewYork-Presbyterian Hospital
Certifications
American Board of Orthopaedic Surgery
Awards
Castle Connolly Top Doctor - 15 Years
Castle Connolly America's Top Doctors, 2014-2020
Castle Connolly Top Doctors in New York Metro Area, 2009-2022
New York Magazine Top Doctors, 2012-2022
Philip D. Wilson, Jr. Teaching Award, 1999
Eastern Orthopaedic Association Founder Award, 1996
Knee Society Award, 1994
Education
Medical: Johns Hopkins University School of Medicine
Residency: Orthopedic Surgery, Hospital for Special Surgery
Fellowship: Hip/Knee Fellowship, Adult Reconstruction, Hospital for Special Surgery
State Licensure
New York, Connecticut
Languages
EnglishFor My Patients
Patient Education
- Your Pathway to Recovery: A Patient's Guide to Total Hip and Knee Replacement Surgery
- Learn why you should choose HSS for your hip or knee replacement.
- Please contact the Patient Education team Monday through Friday between 9:00am and 3:00pm at 212.606.1263 for general questions about your surgery and the educational materials you have received and accessed on the website.
Office Hours, Locations, and Directions
Office Hours:
Monday – Friday, 9:00am – 5:00pm
Tel: 212.606.1674
Fax: 212.472.3713
Office Locations:
Hospital for Special Surgery
535 East 70th Street
New York, NY 10021
[directions]
Helen Hayes Rehabilitation Hospital
51 N Route 9W
West Haverstraw, NY 10993
[directions]
Publications by Dr. Bostrom
Patient Education
Selected Journal Articles
Research
The overall aim of my laboratory efforts continues to be gaining a better understanding of the fundamental principles of bone healing and to use these principles in the development of methods to improve bone healing. Current projects include the use of a multigene assay to quantitatively describe the genetic cascade of growth factors and cytokines during the process of fracture healing. This work will be done in collaboration with Paul Cannon, Ph.D. at Roche Bioscience since he has access to gene chip technology. In addition to this work in the rat fracture model, we will also be collaborating with the scientists at Roche Bioscience in studying the gene expression in a number of human musculoskeletal tissues harvested during total joint arthroplasty procedures.
In collaboration with Nancy Camacho, Ph.D., we are also using Fourier transform infrared microscopy to better define the mineral and organic matrix characteristics of fracture callus. To achieve this goal we have recently developed a fracture model in the mouse and will be utilizing this model to determine the effects of alendronate treatment on the healing normal fractures as well as fractures in OIM mice. My collaboration with Dr. Camacho is also proceeding on developing a FTIR probe to study ultrastructural properties of cartilage and bone in human tissues harvested from total joint arthroplasties performed by me. In the future the use of FTIR methodology may prove to be of significant value in assessing the regeneration of cartilage through tissue engineering in both animal models and clinically. Thus a major thrust this upcoming year will be made with Dr. Camacho to assess the feasibility of using this technology in such a manner.
One of my major development projects over the last several years, in close association with Tim Wright Ph.D. and Marjolein van der Mullen Ph.D., has been the development of an in vivo cyclic loading device in rabbits to study the remodeling process of trabecular bone. This remodeling process has been studied with and without the use of exogenous osteogenic growth factors, and we are currently completing a series of experiments investigating the effects of magnitude, frequency and duration of load on trabecular bone. This work is being partially funded by a generous grant from the Oxnard Foundation and a development and feasibility grant from the NIH. The eventual goal is to improve bone adaptation around total joint implants, and the work will continue to proceed in this direction in the upcoming year with some modification of the loading device currently utilized with the goal of scaling it down to be used in rodents. This modification of the device will be made in collaboration with Dr. Per Aspenberg at the University of Lund in Lund, Sweden. With the anticipated arrival of a micro-CT device at HSS in the upcoming months work on this project as well as other collaborative bone projects will be significantly enhanced.
Clinically, I continue with efforts to establish RSA as outcome measure for total joint arthroplasty. The equipment for performing the studies is on site and we have obtained IRB approval to proceed with these studies. Finally, in the clinical arena, in collaboration with Dr. Kudryck at the New York Blood Center, I hope to be investigating the use of a novel fibrinogen assay to assess the role of the clotting cascade in patients with total hip arthroplasties.
Clinical Trials / Research Studies
Industry Relationships
HSS has a long history of supporting appropriate relationships with industry because they advance HSS's mission to provide the highest quality patient care, improve patient mobility, and enhance the quality of life for all, and to advance the science of orthopedic surgery, rheumatology, and their related disciplines through research and education.
Below are the healthcare industry relationships reported by Dr. Bostrom as of July 13, 2023.
- American Austrian Foundation - Board Member, Research Support
- Hip Society - Board Member
- HS2, LLC - Ownership Interest
- Ines Mandl Foundation - Research Support
- Joint Effort Administrative Services Organization, LLC (“JEASO”) - Ownership Interest- (Through JEASO-minority owner of the Recovery Shop)
- Smith & Nephew - Consultant; Research Support; Royalties
HSS and its physicians make this information available to patients and the public, thus creating a transparent environment for those who are interested in this information. Further, the HSS Conflicts of Interest and Commitment Policy prohibits physicians from collecting royalties on products they develop that are used on patients at HSS. Patients should feel free to ask their HSS physicians questions about these relationships.

