Antiphospholipid Syndrome and the Gut Microbiome – Top 10 Series
- What is APS?
- What is the human microbiome?
- How can the gut microbiome make us susceptible to diseases?
- What are the symptoms of an unhealthy gut microbiome?
- Is there a connection between an unhealthy gut microbiome and antiphospholipid syndrome?
- What are the potential mechanisms by which an unhealthy microbiome can trigger antiphospholipid antibodies?
- Are there specific bacteria or viruses in “unhealthy microbiomes” that may trigger antiphospholipid antibodies?
- If I have antiphospholipid syndrome, can I be tested for an unhealthy microbiome?
- How can I improve my gut health? Are there any treatments being developed for an unhealthy microbiome?
- How can I learn more about the microbiome?
1. What is APS?
Antiphospholipid syndrome (APS) is a systemic autoimmune disorder that causes blood clotting in the veins and arteries as well as pregnancy losses. This is a result of antibodies, known as antiphospholipid antibodies (aPL), that target healthy cells in the body. Sometimes, APS can be associated with other systemic autoimmune disorders including lupus (also known as systemic lupus erythematosus or SLE). For general information on APS, please see our main antiphospholipid syndrome condition webpage.
2. What is the human microbiome?
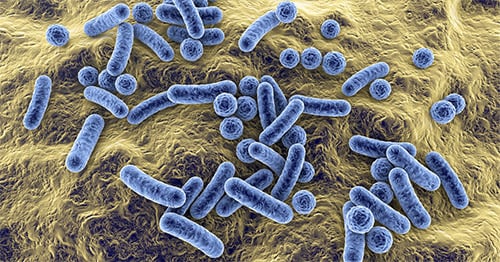
The human microbiome is a collection of bacteria, fungi, viruses, and other types of microbes that exist on various sites of the body, including the gut (digestive tract). These organisms (known as “microbiota”) support the function of human body systems, in particular the immune system. There are approximately 40 trillion bacteria living in the human microbiome. Many of these microbes regulate and train the human immune system. Diet, age, environment, and genetics all contribute to the composition and function of each person’s microbiota. This, in turn determines whether an individual’s microbiome will sufficiently support the immune system or leave the body susceptible to disease as a result of an improperly functioning immune system.
3. How can the gut microbiome make us susceptible to diseases?
The gut microbiome profoundly influences our immune system, and this plays a large role in our susceptibility to diseases. An unbalanced or unhealthy microbiome can weaken the gut barrier and allow gut microbes to leak through and disturb immune and other body functions.
Diet, genes and environmental factors influence the development of the microbiome throughout life, starting as early as during the neonatal (newborn) development. Accumulating environmental triggers, including medication exposures and dietary patterns may result in an unbalanced microbiome, which promotes the development of a dysfunctional immune system.
Autoimmune diseases (when the immune system attacks its own healthy cells) as well as other chronic inflammatory diseases are associated with a decreased diversity of the gut microbiome. This is called “dysbiosis.” Conversely, a healthy microbiome maintains a balanced and diverse collection of microbes and their function, and this contributes to a well-functioning immune system.
4. What are the symptoms of an unhealthy gut microbiome?
There are various gastrointestinal signs and symptoms associated with an unhealthy gut microbiome. Patients with an unhealthy microbiome may experience diarrhea, abdominal pain, and bloating. The microbiome contributes to gastrointestinal disorders such as irritable bowel syndrome and inflammatory bowel disease.
A variety of non-gastrointestinal diseases are also associated with an unhealthy microbiome and linked to body dysfunctions in studies on animals. Besides autoimmune diseases, these include heart disease, metabolic and neurologic disorders. These diseases are also influenced by the microbiome that contributes to the development of diverse signs and symptoms affecting internal organs, such as chest pain, weight gain or difficulties with movement.
5. Is there a connection between an unhealthy gut microbiome and antiphospholipid syndrome?
Although further studies are needed to better understand the role of the microbiome in APS, there are several connections known. Some APS patients carry a less diverse microbiome that is coated by immune molecules called antibodies. In addition, some patients have signs of a leaky gut barrier (without gastrointestinal symptoms), which may allow the immune system outside the gut to be abnormally stimulated by gut microbes. In studies on mice, an “unhealthy microbiome” has been shown to trigger antiphospholipid antibodies (aPL) that could be prevented by certain antibiotics. In addition, mice that have been bred to be predisposed to APS and which are then colonized with a particular human gut microbe, developed increased levels of aPL and blood clots.
6. What are the potential mechanisms by which an unhealthy microbiome can trigger antiphospholipid antibodies?
When present, an “unhealthy microbiome” can induce harmful antibodies that attack healthy cells in the body, causing autoimmunity in people who have a genetic predisposition. In patients with APS, an unhealthy microbiome may release antigens that appear similar to a normal protein in the blood: Beta-2-glycoprotein-I (β2GPI). In some people, these released antigens can confuse the immune system and trigger the production of a harmful antibody against this β2GPI protein. This is the so-called anti-Beta-2-glycoprotein-I (aβ2GPI) antibody. This “confusion” process is called “cross-reactivity” or molecular mimicry. These self-reactive antiphospholipid antibodies (aPL) subsequently contribute to serious clinical signs and symptoms seen in APS patients, such strokes, heart attacks or trouble breathing or speaking due to blood clots in the lungs.
7. Are there specific bacteria or viruses in “unhealthy microbiomes” that may trigger antiphospholipid antibodies?
Several pathogens (bacteria or viruses invading from the outside) have previously been associated with antiphospholipid antibodies, but which do not necessarily lead to a person having antiphospholipid syndrome. Microbes that live inside the body and which could trigger persistent aPL, have not yet been studied in detail.
For example, several bacterial microbes within human microbiomes produce cardiolipin, a lipid that is frequently attacked by the immune system in people with APS. But there have been no investigations yet to determine whether or not those bacteria directly contribute to a person contracting the disease.
However, in a recent study, researchers uncovered that a bacterium called Roseburia intestinalis (which is commonly found in the human gut microbiome) may trigger an immune response associated with APS in patients who are genetically predisposed to the disease. Roseburia intestinalis carries the above-mentioned proteins that are similar to parts of the blood protein β2glycoprotein-I. Natural immune responses to this bacterium may then elicit an autoimmune response by cross-reactive mechanisms that sustain aPL production in predisposed individuals.
Supporting this possibility, higher levels of immune responses to Roseburia intestinalis were correlated with increased aPL levels in APS patients. Therefore, if we can reduce the number of these organisms in a patient’s microbiome, we might reduce the "confusion" process and thus reduce the formation of aPL.
8. If I have antiphospholipid syndrome, can I be tested for an unhealthy microbiome?
Currently, APS patients are not tested for “unhealthy microbiome” in the clinical setting (the doctor’s office or hospital), however, such tests are being researched. Researchers are in the process of testing various ways to monitor microbiome health and signs for disease, for instance with a so-called “smart toilet.” This is a device that can be affixed to a toilet to monitor urine and stool for signs of disease.
Others have created at-home microbiome tests, which are difficult to interpret across diverse populations. These tests are therefore relatively unreliable for individual subjects. Also, they are not tailored to APS patients. More research is being conducted to find methods to test for “unhealthy microbiomes” in general and for APS patients specifically.
9. How can I improve my gut health? Are there any treatments being developed for an unhealthy microbiome?
Treatments for an "unhealthy microbiome" are being developed, however, the microbiome is an evolving area of research and treatments for any disease will take time. They require carefully designed studies to account for the variability of microbiomes across people.
Dietary interventions have been one area of focus to temporarily restore a healthy microbiome. However, they may have to be tested in a personalized fashion, as everyone`s microbiome and body functions can respond differently to the same kind of diet, for instance, to a sugar load. Some dietary components have more general effects on the gut. Dietary fibers can enforce the gut barrier. A particular fiber-rich diet, so-called resistant starch, was shown to mitigate lupus, a condition related to APS, in a mouse model. This diet strengthened the gut barrier and prevented disease-promoting gut microbes from getting into internal organs. If this type of diet might be beneficial for subsets of APS or lupus patients will first have to be tested. A fiber-rich, plant-based diet, however, can generally be recommended for subjects who lack fibers in their diet.
Additionally, fecal transplants have been used as a microbiome therapy to restore a diverse microbiome by introducing healthy bacteria to the gut. However, fecal transplants can sometimes be associated with serious side effects, especially in patients with a compromised immune system. Patients with a suppressed immune system can develop infections from pathogens that are inadvertently introduced within the fecal transplant. Current efforts are aimed at thoroughly screening and standardizing the microbiomes to be transplanted into patients. While this approach has proven to be effective in certain gut and some non-gut diseases, these studies were still small and have not yet been performed in APS patients.
Finally, a variety of other, more tailored treatment approaches targeting the microbiome are being tested at early stages. For instance, specific depletions or additions of individual microbes are being developed by several companies and research groups. It is unclear if these personalized approaches turn out to become future treatment options for patients with autoimmune diseases.
10. How can I learn more about the microbiome?
Below are several websites and podcasts that provide more information about the microbiome:
Antiphospholipid Syndrome (APS) Patient Stories
References
- Antiphospholipid Syndrome (APS). (n.d.). HSS. Retrieved April 22, 2021, from https://www.hss.edu/condition-list_antiphospholipid-syndrome.asp.
- Gut Microbiome Implicated in Antiphospholipid Syndrome [Fact sheet]. (2019, June 18). HSS. Retrieved April 22, 2021, from https://news.hss.edu/gut-microbiome-implicated-in-antiphospholipid-syndrome/.
- Gupta, A., Saha, S., & Khanna, S. (2020). Therapies to modulate gut microbiota: Past, present and future. World journal of gastroenterology, 26(8), 777–788. https://doi.org/10.3748/wjg.v26.i8.777.
- Kolodziejczyk AA, Zheng D, Elinav E. Diet-microbiota interactions and personalized nutrition. Nat Rev Microbiol. 2019 Dec;17(12):742-753.
- Manfredo Vieira, S., Hiltensperger, M., Kumar, V., Zegarra-Ruiz, D., Dehner, C., Khan, N., Costa, F., Tiniakou, E., Greiling, T., Ruff, W., Barbieri, A., Kriegel, C., Mehta, S. S., Knight, J. R., Jain, D., Goodman, A. L., & Kriegel, M. A. (2018). Translocation of a gut pathobiont drives autoimmunity in mice and humans. Science (New York, N.Y.), 359(6380), 1156–1161. https://doi.org/10.1126/science.aar7201
- The Microbiome [Fact sheet]. (n.d.). Harvard T.H. Chan School of Public Health. Retrieved April 22, 2021, from hsph.harvard.edu/nutritionsource/microbiome/.
- Ruff, W. E., Dehner, C., Kim, W. J., Pagovich, O., Aguiar, C. L., Yu, A. T., Roth, A. S., Vieira, S. M., Kriegel, C., Adeniyi, O., Mulla, M. J., Abrahams, V. M., Kwok, W. W., Nussinov, Erkan, D., Goodman, A. L., & Kriegel, M. A. (2019). Pathogenic Autoreactive T and B Cells Cross-React with Mimotopes Expressed by a Common Human Gut Commensal to Trigger Autoimmunity. Cell host & microbe, 26(1), 100–113.e8. https://doi.org/10.1016/j.chom.2019.05.003.
- Ruff, W. E., Greiling, T. M., & Kriegel, M. A. (2020). Host-microbiota interactions in immune-mediated diseases. Nature reviews. Microbiology, 18(9), 521–538. https://doi.org/10.1038/s41579-020-0367-2.
- Ruff, W. E., Vieira, S. M., & Kriegel, M. A. (2015). The role of the gut microbiota in the pathogenesis of antiphospholipid syndrome. Current rheumatology reports, 17(1), 472. https://doi.org/10.1007/s11926-014-0472-1.
- Zegarra-Ruiz D. F., El Beidaq, A., Iñiguez, A. J., Lubrano Di Ricco, M., Manfredo Vieira, S., Ruff, W. E., Mubiru, D., Fine, R. L., Sterpka, J., Greiling, T. M., Dehner, C., & Kriegel, M. A. (2019). A Diet-Sensitive Commensal Lactobacillus Strain Mediates TLR7-Dependent Systemic Autoimmunity. Cell host & microbe, 25(1), 113–127.e6. https://doi.org/10.1016/j.chom.2018.11.009.

