Antiphospholipid Syndrome and Lung Disease
Top 10 Points Patients Should Know About How Antiphospholipid Syndrome Can Affect Their Lungs

- What is antiphospholipid syndrome (APS)?
- What is the structure (anatomy) of lungs?
- What are different types of lung (pulmonary) disease in APS, and how common are they?
- What is pulmonary embolism and how does it present?
- What is diffuse pulmonary hemorrhage and how does it present?
- What is pulmonary hypertension and how does it present?
- What tests are used to diagnose APS-related lung disease?
- How do you prevent or treat pulmonary embolism?
- How do you treat diffuse pulmonary hemorrhage?
- How do you treat pulmonary hypertension?
-
What is antiphospholipid syndrome (APS)?
Antiphospholipid syndrome (APS) is a systemic autoimmune disease in which the person's immune system develops autoantibodies (antiphospholipid antibodies [aPL]) that bind to certain molecules and proteins on cell surfaces; thus, predisposing patients to blood clots. In addition to blood clots, APS patients may develop pregnancy complications and problems not related to blood clots such as thrombocytopenia (low platelet counts). Three common tests used to determine aPL are lupus anticoagulant (LA), anticardiolipin antibody (aCL), and anti-Beta-2-glycoprotein-I antibody (aβ2GPI).
-
What is the structure (anatomy) of lungs?
Lungs are divided into different lobes. The right lung has three lobes, while the left lung has only two lobes. Lungs are covered by a protective membrane called the pleura and separated by the mediastinum, which contains the heart.
There are two kinds of lung structures: parenchymal and non-parenchymal.
- The lung parenchyma, is responsible for gas exchange and includes alveolar ducts and alveoli (small air sacs where oxygen exchange takes place).
- Non-parenchymal lung structures consist of the bronchial tree (trachea, bronchi), interlobular septa, and pulmonary vessels.
- Lung circulation depends of three types of blood vessels (see image):
- Two pulmonary arteries (one left and one right), which carry deoxygenated blood from the right side of the heart to the lungs to be oxygenated (distinct from other arteries in the body that carry oxygenated blood).
- Four pulmonary veins (two for each lung), which carry oxygenated blood from the lungs to the left side of the heart.
- Bronchial arteries, provide oxygenated blood to the lungs and the bronchial veins participate in the venous drainage (deoxygenated blood).
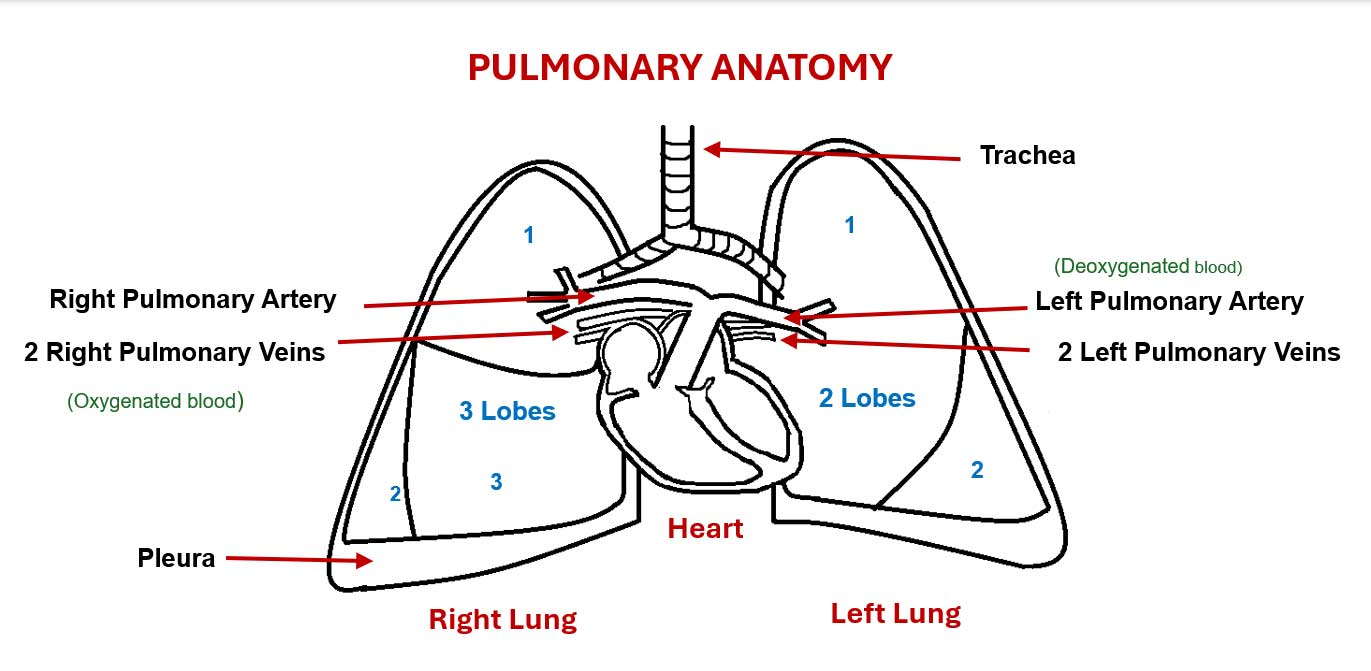
Image. Structures of the pulmonary anatomy: trachea, lungs, pleura, pulmonary arteries and veins (created by Marcela Avila Andrade).
-
What are the different types of lung disease in APS, and how common are they?
- Pulmonary Embolism (defined below):
- Pulmonary (lung) embolism is the most frequent pulmonary manifestation in APS. The frequency varies between studies, ranging from 10% to 40% of APS patients. In up to 50% of patients, pulmonary embolism presents with blood clots within the veins, mainly in lower limbs (deep vein thrombosis [DVT]).
- Diffuse Alveolar Hemorrhage (DAH) (defined below):
- Diffuse alveolar hemorrhage (bleeding) may develop in 2% to 12% of APS patients.
- Pulmonary Hypertension (PHTN) (defined below):
- Pulmonary hypertension may develop in 2% to 4% of APS patients.
- Others: Relatively rare other lung involvements in APS include:
- Acute respiratory distress syndrome (ARDS) has been rarely described in the context of APS (less than 1% of APS patients). ARDS is an acute inflammatory pulmonary response that may be triggered by many different causes (such as infections, emboli, or trauma), and characterized by flooding of the alveoli with fluid that produces alterations in gas exchange. ARDS is usually part of catastrophic APS (CAPS), which is the most severe form of APS with multiple clots in small, medium, and large blood vessels.
- Fibrosing alveolitis: A condition characterized by thickening of the tissue around the alveoli and the formation of scar tissue that produces a progressive and irreversible loss of lung function to oxygenate the blood. There are few cases of fibrosing alveolitis reported, therefore the association with APS is not clear.
- Postpartum Syndrome: A clinical picture consisting of spiking fevers, pleural chest pain, and dyspnea in women during the postpartum period (after delivery), with chest radiographs showing pleural effusions (fluid accumulation) and patchy infiltrates (dense white shadows). Based on a few cases reported, postpartum syndrome has been considered as a form of CAPS in APS patients.
-
What is pulmonary embolism and how does it present?
Pulmonary embolism (blockage of the pulmonary artery generally by a clot) is the main type of lung involvement in APS and may be the first manifestation of the disease. The occlusion of the pulmonary artery by a blood clot prevents the normal passage of blood to the lungs; the clots may come from another part of the body, usually from lower limbs. Recurrent pulmonary emboli increase the risk of developing pulmonary hypertension (further discussed below).
The characteristic symptoms of pulmonary embolism are:
- Sudden onset breathlessness.
- Fast heartbeat.
- Chest pain.
- Loss of consciousness, hypotension (low blood pressure), and cyanosis (purple color of the skin) indicate a more severe disease.
-
What is diffuse pulmonary hemorrhage and how does it present?
Diffuse pulmonary hemorrhage (bleeding) also known as diffuse alveolar hemorrhage (DAH), caused by leakage of blood from the alveolar capillaries (microvessels of the alveolar sacs) into the intraalveolar space. Pulmonary hemorrhage in APS occurs due to inflammation and/or blood clots in the microvessels of the lung.
Diffuse alveolar hemorrhage is characterized by laboratory features such as anemia and hypoxemia (low levels of oxygen in the blood), bilateral pulmonary infiltrates (white shadows on X-ray images of the lung due to involvement of the alveoli), and respiratory symptoms (described below).
Diffuse alveolar hemorrhage can occur in the context of many other autoimmune diseases (such as systemic lupus erythematosus) or infections. Therefore, other underlying problems should be excluded, since DAH is a rare manifestation in APS.
The characteristic symptoms of DAH are:
- Cough
- Breathlessness
- Hemoptysis (bleeding with coughing)
- Pleuritic chest pain
- Acute respiratory failure (inability of the lungs to exchange gases) in severe cases.
-
What is pulmonary hypertension and how does it present?
Pulmonary hypertension (PHTN) is a chronic and progressive disease, characterized by sustained elevation of pressure in the blood vessels of the lungs, which causes the heart to work harder than normal to try to pump blood to the lungs, which can damage the heart.
Pulmonary hypertension is classified into five groups depending on the underlying mechanism. In APS, the main cause of pulmonary hypertension is recurrent pulmonary embolism. Antiphospholipid syndrome patients can develop three types of pulmonary hypertension:
- Pulmonary arterial hypertension
- Pulmonary hypertension due to left heart disease
- Secondary to systolic dysfunction (the heart cannot effectively contract), diastolic dysfunction (the heart cannot effectively relax after the contraction), or valvular (structure of the heart that opens and closes, allowing or not the passage of blood) disease.
- Chronic thromboembolic pulmonary hypertension – CTEPH
- The recurrent blood clots cause changes in the walls of the pulmonary arteries with the development of insitu microthrombosis (thrombi within the microvessels), which causes an increase in pressure within these blood vessels, and the secondary development of pulmonary hypertension.
The characteristic symptoms of pulmonary hypertension are:
- Breathlessness at the beginning with physical activity and then at rest.
- Fatigue
- Chest pain
- Dry cough
- Cyanosis (defined above) due to low oxygen levels
- Dizziness or loss of consciousness
- Swelling of lower limbs and abdomen due to fluid accumulation in more advanced stages.
-
What tests are used to diagnose APS-related lung disease?
A detailed medical history and physical examination are the initial steps in APS diagnosis. After then, the majority of the lung problems in APS patients can be detected by one or more of the following:
- Laboratory tests, including a marker, D-dimer, which can predict the likelihood of blood clots.
- Standard chest x-ray may reveal bilateral infiltrates (described above), which may be better visualized with computed tomography (CT).
- Computed tomography pulmonary angiography and ventilation-perfusion scanning are the most validated imaging tools for the diagnosis of pulmonary embolism, as they allow visualization of clots in the blood vessels of the lungs.
- Ultrasound studies such as Doppler ultrasound allows the visualization of clots in different parts of the body, or ultrasound of the heart (echocardiography) is usually the initial approach in patients with suspected pulmonary hypertension. If indirect signs of pulmonary hypertension are evident, cardiac catheterization should be performed to diagnose pulmonary hypertension.
- Right heart catheterization (RHC) allows diagnosing pulmonary hypertension. It involves passing a catheter (thin tube) usually from the neck or groin to the right side of the heart to measure the pressure in the pulmonary artery.
- Bronchoscopy (visualization of the airways by introducing a device called a bronchoscope) and bronchoalveolar lavage (sample collected after introducing and washing the airways with saline) are sometimes necessary to confirm the underlying problem, which are also important to rule out infections. Bronchoalveolar lavage (BAL) is important for diffuse alveolar hemorrhage diagnosis, showing a hemorrhagic appearance (red color) of the fluid on direct visualization, and in confirmatory tests greater than 20% of hemosiderin-laden macrophages (cells responsible for ingesting and destroying harmful products loaded with a red cell degradation product) are observed.
- Lung biopsy should be considered if the diagnosis has not been made with any of the tests discussed above. Lung biopsy consists of removing a small portion of the lung tissue for microscopic examination, which may be sometimes useful for diagnosing diffuse alveolar hemorrhage when BAL is not helpful; and also useful for excluding any other diseases with lung involvement.
-
How do you prevent or treat pulmonary embolism?
General measures to prevent pulmonary embolism in antiphospholipid antibody (aPL)-positive patients include:
- If you have a long trip, the risk of blood clot is higher, so it should be prevented by wearing compression elastic stockings and avoid popliteal pressure while sitting. In addition, you can walk or extend your legs on plane or train trips and make stops on car trips at least every hour.
- Immobilization due to surgery or fractures increases the risk of thrombi, therefore it is important to tell the surgeon about you have aPL and/or APS so that they can take measures before and after surgery.
- Avoid the use of estrogen containing birth control pills, which increase the risk of blood clots.
- Physical exercise and eating healthy to prevent/control cardiovascular risk factors such as high blood pressure, high cholesterol, diabetes, and obesity.
- Smoking cessation is crucial.
If you are receiving blood thinners (defined below) such as warfarin, for history of a previous blood clot, it is essential maintaining your target INR (International Normalized Ratio, an index that measures the time takes for blood to clot) levels.
Treatment of pulmonary embolism in APS patients is the same as the treatment of pulmonary embolism for other causes in non-APS patients. Management of acute clot requires blood thinners (anticoagulant drugs – medications that prevent clotting), initially with subcutaneous or intravenous blood thinners, and then maintenance therapy with oral blood thinners, such as warfarin. Long-term (possibly lifelong) treatment is generally needed to prevent recurrence of blood clots.
In case of pulmonary embolism with hemodynamic instability (low blood pressure with decreased blood flow), the thrombolysis (removal of thrombus with drugs administration), pulmonary embolectomy (removal of thrombus through surgery) or catheter-directed embolectomy (a less invasive approach where catheters are directed through veins and devices are deployed to suction clots out of the pulmonary circulation) are options. Anticoagulation is the gold-standard treatment and will be given in addition to any other potential procedure.
Currently, there are other oral anticoagulants known as direct oral anticoagulants (DOACs) with a different mechanism of action than warfarin that do not require INR controls, however their efficacy and safety in not well-proven in APS.
-
How do you treat diffuse pulmonary hemorrhage?
Treatment of diffuse pulmonary hemorrhage (DAH) should be aggressive and started as soon as possible. The administration of corticosteroids (a medication with multiple effects including metabolic, anti-inflammatory, and immunosuppressive actions) usually intravenously in high doses daily for three to five days is the most important and initial step.
After the administration of corticosteroids, it is essential to start immunosuppressive drugs (medications that suppress immune system function) to avoid relapses. Rituximab and mycophenolate mofetil are immunosuppressive drugs that are useful in the treatment of DAH based on case reports and small case series.
In cases where there is no response to rituximab or mycophenolate mofetil, other treatments may be tried, such as:
- Intravenous immunoglobulins (antibodies obtained from donor plasma, which are used to block inflammation).
- Plasmapheresis – This is a procedure in which blood is extracted from the patient, blood cells are separated from the plasma (liquid part of the blood) and then returned to the body, and the plasma is discarded or replaced with another fluid.
-
How do you treat pulmonary hypertension?
The goals of treatment for pulmonary hypertension (PHTN) are to improve symptoms and prolong survival. The management is based on the following measures:
- Medical Treatment:
- Blood thinners: Antiphospholipid syndrome patients with secondary PHTN generally receive blood thinners to avoid new blood clots, since this is the main cause of PHTN in these patients.
- Vasodilatory drugs such as calcium antagonists, endothelin receptor antagonists, phosphodiesterase-5 inhibitors, prostacyclin analogs. These medications, generally used in combination, act by opening blood vessels in the lungs and improving blood flow.
- Riociguat is a specific drug used in the treatment of patients with PHTN when they are not candidates for surgical treatment due to the distal and inaccessible nature of the lesions or to comorbidities. It acts by relaxing and opening the pulmonary blood vessels.
- Surgical Treatment
- Pulmonary endarterectomy is the treatment of choice for patients with PHTN. It consists of removing the thrombus from the pulmonary arteries to restore blood flow to the lungs.
- Others:
- Oxygen therapy in cases of heart failure (inability of the heart to pump blood to the body) or hypoxemia (defined above).
Posted: 6/28/2024
Authors
Marcela Avila Andrade, MD
Academic Visitor, Department of Rheumatology, Hospital for Special Surgery
Reyhan Kose Cobanoglu, MD
Academic Visitor, Department of Rheumatology, Hospital for Special Surgery
Lindsay Lief, MD
Associate Professor of Clinical Medicine, Pulmonary and Critical Care Medicine
Weill Cornell Medicine
Attending Rheumatologist, Hospital for Special Surgery
Professor of Medicine, Weill Cornell Medical College
Related articles
Antiphospholipid Syndrome (APS) Patient Stories
References
- Arachchillage D, Pericleous C. Evolution of Antiphospholipid Syndrome. Semin Thromb Hemost. 2023; 49:295–304.
- Cohen H, Cuadrado MJ, Erkan D, et al. 16th International Congress on Antiphospholipid Antibodies Task Force Report on Antiphospholipid Syndrome Treatment Trends. Lupus. 2020; 29:1571-1593.
- Erkan D. Expert Perspective: Management of Microvascular and Catastrophic Antiphospholipid Syndrome. Arthritis Rheumatol. 2021;73 :1780-1790.
- Espinosa G, Cervera R, Font J. The lung in the antiphospholipid syndrome. Ann Rheum Dis .2002;61:195–198.
- Ford J, Roubey R. Pulmonary Manifestations of the Antiphospholipid Antibody Syndrome. Clin Chest Med .2010; 31: 537–545.
- Gaspar P, Sciascia S, Tektonidou MG. Epidemiology of antiphospholipid syndrome: macro- and microvascular manifestations. Rheumatology .2024;63: SI24-SI36.
- Itoh H, Nishio M, Hatabu H. Architecture of the lung. J Thorac Imaging. 2004; 19:221–227.
- Iverson R, Gomez J. Deep Venous Thrombosis Prevention and Management. Clin Plastic Surg 40. 2013; 389–398
- Kanakis M.A, Kapsimali V, Vaiopoulos A.G, Samarkos M. The Lung in the spectrum of antiphospholipid síndrome. Clin Exp Rheumatol.2013; 31: 452-457.
- Maioli G, Calabrese G, Chighizola C. Lung disease in Antiphospholipid syndrome. Semin Respir Crit Care Med. 2019; 40:278–294.
- Porta S, Castro Oliveira de Andrade D, Erkan D. Controversies in the Management of Antiphospholipid Syndrome. J Clin Rheumatol. 2023;29: e107–e112.
- Rosen K, Raanani E, Agmon-Levin N. Chronic thromboembolic pulmonary hypertension in patients with antiphospholipid syndrome: Risk factors and management. J Heart Lung Transplant. 2022; 41:208−216.
- Stojanovich L. Pulmonary manifestations in antiphospholipid syndrome. Autoimmunity Reviews .2006; 344–348.
- Tektonidou M, Andreoli L, Limper M. EULAR recommendations for the management of antiphospholipid syndrome in adults. Ann Rheum Dis. 2019; 78:1296–1304.
- Wells A, Denton C. (2004). Hadbook of systemic autoinmune diseases. Pulmonary involvement in Systemic Autoinmune Diseases. Asherson R. 2004; 137-145. Elsevier.


