Eye Problems in Lupus
Lupus (systemic lupus erythematosus) can affect multiple organs in the body. This can include any of the structures in your eye.
Introduction: The eye’s anatomy and function
The eye is a globe that is filled with a gelatinous material. The lining of the globe consists of several layers. From the outside to inside, the eye’s layers are the conjunctiva, the sclera, the uvea, and the retina. The different layers also acquire different names, depending on whether we’re talking about the front of the eye, or the rear of the eye. For example, the cornea is the part of the sclera that covers the front part of the eye. The iris, which is the colored part of the eye, is the name we give to the uvea in the front part of the eye, while the choroid, which is the vascular part of the eye, is the name we give to the uvea in the back of the eye.
The pupil is the black hole in the middle if your iris – it is actually an opening through which light enters. The iris and its associated ciliary body, all part of the uvea, are responsible for how big or small the iris becomes, in response to how much light there is. The more light there is, the smaller the iris becomes. Conversely, the less light there is, the larger the iris becomes. If you are into photography, you’ll be somewhat familiar with this concept, as cameras operate in the same way.
The retina – the back part of the eye – is where the light that comes through the pupil is projected. The resulting image is interpreted by the optic nerve.
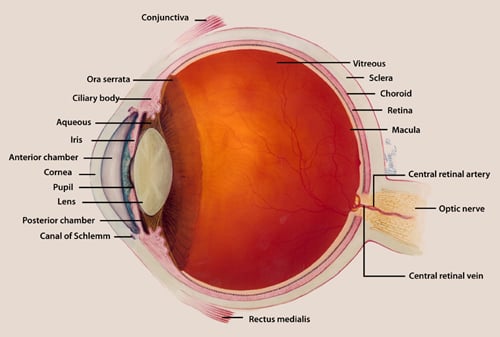
Diagram of the anatomy of the eye. [Courtesy of the National Eye Institute]
Disorders extrinsic to the eye
These conditions affect the outer part of the eye, such as the eyelids and tear glands.
Dry eyes/Sjogren’s
Sjogren’s syndrome is a syndrome of dryness, often involving the eyes. The problem here is that the tear glands are not producing enough tears. Patients with lupus often also have dry eyes, whether they strictly meet criteria for Sjogren’s syndrome or not. Often the sensation is one of having grit in your eyes; sometimes the opposite can occur, where you might be tearing excessively.
Discoid lupus
Discoid lupus is a form of lupus that can involve the skin. This can sometimes involve the eyelid.
Disorders intrinsic to the eye
These conditions, which affect inner parts of the eye, such as the iris, the retina, or the optic nerve, are rare in lupus, though can occur.
Scleritis/episcleritis
When the outermost layers of the eye are inflamed, the eye can appear very red; sometimes it is painful. Blurred vision can occur.
Choroiditis
In lupus patients, when the uvea is inflamed (uveitis), it is typically in the form of choroiditis, or inflammation of the choroid – the vascular, posterior part of the uvea, which is the blood supply of the retina. The blood vessels can be disrupted, sometimes causing a retinal detachment. This is extremely rare, occurring usually when systemic disease is also active.
Retinal vasculitis
Inflammation of the blood vessels is known as vasculitis. In people with lupus, the blood vessels that supply the retina can become inflamed. This causes the blood flow to be compromised, leading to alterations in vision. Just like choroiditis, this often correlates with active lupus disease elsewhere, so that when systemic disease is well-controlled, this complication is extremely rare. (Learn more about vasculitis as it relates to lupus.)
Central retinal artery occlusion
In lupus patients who also have antiphospholipid antibody syndrome, clots can develop in many different body parts, and the retinal artery is not exempt. This causes sudden loss of vision.
Optic neuritis
The optic nerve itself can sometimes be inflamed in lupus, or it can be affected when the blood vessels supplying the nerve are themselves inflamed (that is, ischemic optic neuropathy). This can lead to a change in vision, or even vision loss.
Eye issues induced by lupus medications
Hydroxychloroquine retinal toxicity
Hydroxychloroquine is really the backbone of the treatment of systemic lupus. In some cases, when the dose of hydroxychloroquine exceeds 5 mg/kg/day and the patient has been on it for less than 10 years, we can start to see the medication deposit in the retina. If you see your ophthalmologist yearly and they are aware that you are on this medication, they will be able to detect these changes before you appreciate any change in your vision. At that point we have to discontinue the medication.
Side effects of glucocorticoids
If you’ve ever been on systemic steroids, then you know that this comes with a large list of potential side effects. This includes glaucoma, where the pressure in the eye is elevated beyond normal. Left uncorrected, this causes damage to the optic nerve and can lead to vision loss. Not to worry, if you see your eye doctor regularly, they routinely check your eye pressure (that’s what they’re doing when they use that fancy instrument that blows a puff of air directly at your eye).
Cataracts are another potential side effect of systemic steroids. They do occur even in the absence of steroid use though. The lens becomes cloudy with deposits. This typically evolves slowly, so that there is a gradual blurring of vision. Cataract removal is very often successful and uncomplicated. (Learn more about side effects of steroids and how to reduce them.)
Conclusion
The eyes is a complex organ with many moving parts that can be affected by lupus in different ways. The most common condition is dryness, which can generally be managed with supportive measures. Lupus medications can affect ocular health, so regular ophthalmology visits are a must for the lupus patient. Thankfully, the other, more vision-threatening conditions, are exceedingly rare.
The SLE Workshop at HSS
Learn more about the HSS SLE Workshop, a free support and education group held monthly for people with lupus and their families and friends.

