Hip Arthroscopy and Other Treatments for Hip Conditions
This article is composed of three sections:
Hip arthroscopy is one of various forms of surgical treatments for hip conditions. To better understand the following discussion of these treatments, it is useful to first get an overview of the anatomy of the hip.
What is the anatomy of the hip joint?
The hip joint is the ball-and-socket joint. The head of the femur (thighbone) forms the ball, and the acetabulum forms the socket. Articular cartilage covers both. While the cartilage covers the entire head of the femur, the acetabulum cartilage is in the shape of a horseshoe with a depression (fossa) in the center of the socket. This fossa contains soft tissue and a ligament connecting the femoral head to the socket.
The socket has a rim of rubbery fibrocartilage called the labrum. The labrum acts as a gasket, sealing in fluid and helping to deepen the socket. The function of the hip labrum is analogous to that of the knee meniscus and shoulder labrum. The entire joint is covered with a tough capsule to contain the joint fluid and maintain cartilage lubrication and nutrition.
In addition, numerous tendons surround the hip, as well as bursae, which are lubrication "cushions" where soft tissues glide over bony prominences.
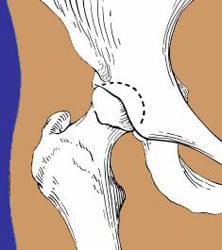
Illustration of hip joint
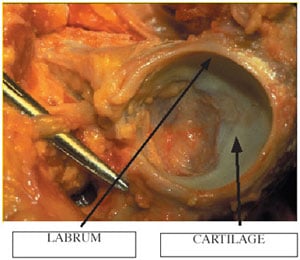
Labrum and cartilage
What are the pathologic conditions that affect the hip joint?
Congenital Abnormalities
For the hip to last a lifetime, the anatomy must be normal along with the absence of catastrophic problems such as trauma or infection. Hip dysplasia refers to a hip that does not develop properly because of congenital dislocation or if the femoral head is not fully seated in the acetabulum. Degenerative changes can occur very early in life; the greater the abnormalities, the sooner symptoms may occur.
Dysplasia can cause arthritis (loss of cartilage) because the shallow socket creates inadequate contact between the ball and socket. The overloaded cartilage can wear away if this situation is not corrected. In addition, the labrum (rim) is often torn, because of the high loads to which it is subjected in trying to maintain coverage of the head.

Dysplastic hip with poor head coverage
Developmental Abnormalities
Certain conditions may occur during childhood and adolescence. These include: Perthes disease (arrest of blood flow to the femoral head) and slipped capital femoral epiphysis (slippage of the cartilage growth plate in the femoral head). These conditions lead to abnormalities of the femoral head anatomy.
If the femoral head is left squared, enlarged, or tilted, early arthritis and labral tears may occur. If the head is left displaced on the femoral neck, an impingement may occur. Impingement means that the femoral neck hits the rim of the socket prematurely during flexion which leads to decreased range of motion, labral tears and ultimately arthritis.
Trauma
The anatomy may be completely normal, but abnormal loads or positions may cause trauma to the joint. Depending upon the severity, the bone may fracture, the articular cartilage may be cracked or shear off either on the head or socket, or the labrum may be torn.
Degenerative Conditions
In the absence of trauma or congenital defects, the hip may simply wear out as we age. These conditions include arthritis (loss of cartilage) or labral tears.
What are the treatment options for conditions that affect the hip joint?
Conservative Measures
Non-operative measures should always be considered first. Rest, behavior modification, physical therapy, and nonsteroidal anti-inflammatory drugs may alleviate reversible disorders. For persistent hip pain, the correct diagnosis must be made. A skilled physician should be able to determine whether the pain is from the hip and not radiating from the lower back or abdomen.
It can be very difficult to differentiate between "intra-articular" (inside the joint) problems such as labral tears, cartilage damage, and arthritis versus "extra-articular" (outside the joint) problems such as tendinitis or bursitis. Corticosteroid injections can be placed into the joint or around bursae and tendons to:
- Confirm the diagnosis: The steroid is mixed with Marcaine, a local anesthetic.
- Provide longer lasting relief by reducing inflammation.
High-resolution MRI scans are indispensable for visualizing bone and soft tissues to help confirm the correct diagnosis.
Surgical Treatments
The type of surgery depends upon the degree of damage, age of the patient, and natural history of the disorder. For hip disorders the options include:
- Hip Arthroscopy
- Osteotomy
- Fusion (Arthrodesis)
- Arthrotomy
- Total Hip Replacement
Hip arthroscopy – Hip arthroscopy has been slower to evolve than arthroscopy of other joints such as the knee or shoulder. The difficulty is that the hip joint is much deeper in the body and therefore harder to access.
To perform the arthroscopy adequately, it is necessary to use traction to distract the joint under anesthesia. This distraction temporarily opens the space between the ball and socket by approximately one-half inch. This space is necessary to insert the scope and small instruments without damaging the labrum and cartilage. While this is possible under general anesthesia, we prefer epidural anesthesia, which provides muscle relaxation and complete pain relief but does not require a tube to be inserted in the airway, resulting in a much safer outcome. Fluoroscopy (X-ray) is used during the case to ensure that the instruments and scopes are inserted properly.
The instruments are inserted through two tiny skin incisions. Occasionally, a third or fourth incision may be required depending upon the procedure. Excellent visualization of the entire joint is possible.
Through the second opening (portal) instruments are inserted to shave tissue, cauterize structures, or remove pieces. On occasion, holes may be drilled into patches of bare bone where the cartilage has been lost. This technique, called "microfracture" or "picking" incites localized bleeding and encourages the formation of fibrocartilage (repair cartilage). Saline is pumped through the joint during the procedure to improve visualization and flush out debrided tissue.

Traction creates space for instrument insertion

Cleaning away torn cartilage
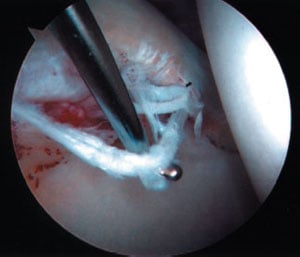
Torn labrum at rim of socket

Removal of loose body from inside the hip
Once the case is finished, the hip may be injected with local anesthetic to decrease postoperative pain and facilitate discharge from the hospital. The procedure is usually done on an outpatient basis. Patients are usually discharged on crutches but can often return to full weight bearing after a few days. Physical therapy may be used during the postoperative period to increase range of motion and strength. It may be necessary to protect weight bearing for as long as six weeks following the procedure if the microfracture technique is used.
It should be noted that while the procedure has vastly improved the ability to treat certain hip disorders with minimal surgical trauma, it is not always an appropriate replacement for other larger operations. If the hip has severe degeneration, total hip replacement may be the only procedure that will provide long-term pain relief. Conversely, in younger patients with skeletal deformities ( i.e. dysplasia, impingement) hip arthroscopy will usually provide relief. But the relief may be short-lived because the underlying pathologic condition has not been corrected.
Osteotomy – Osteotomy (cutting the bone) is a technique were the anatomy of the femur or socket is altered to relieve pain and prolong survival of the joint by reducing the abnormal loads on the cartilage.
Fusion – Fusion (arthrodesis) makes the hip permanently stiff by obliterated the joint via bone bridging across the joint. This procedure was performed much more frequently in the past and is still appropriate in certain conditions, such as severe arthritis of one hip in a young person.
Arthrotomy – Arthrotomy (opening the joint) is a procedure where the joint is opened to clean out bone spurs, loose bodies, tumors, or to repair fractures.
Total Hip Replacement – Total hip replacement is extremely effective at relieving pain and restoring function as well as range of motion. But, it is an artificial joint and should be performed only if other "joint saving" procedures are not appropriate.
Learn more about the HSS Arthritis Service.

