Magnetic Resonance (MR) Neurography
Until recently, precisely localizing the site(s) of peripheral nerve damage was difficult, which made it challenging for doctors to accurately diagnose and treat peripheral nerve disorders. At HSS, we have optimized a specialized MRI technique called magnetic resonance (MR) neurography to localize abnormalities of nerves from the skull base to the tip of the toes.

Schedule an
MR neurography
appointment
Call 212.774.7296
Patients with a wide range of conditions that affect the nerves can now be more quickly and accurately diagnosed.
What is MR neurography?
MR neurography, also known as peripheral nerve MRI, uses high-resolution techniques to visualize nerves throughout the body. A radiologist who specializes in nerve imaging reviews the images to detect abnormal features of the nerve that may indicate injury or inflammation, such as increased brightness or size. By localizing and characterizing nerve abnormalities, MR neurography aids in the diagnosis and management of various conditions.
Specially trained HSS radiologists work closely with referring physicians to determine the appropriate imaging exams for diagnosis and treatment planning.
Can an MRI show nerve damage?
Conventional MRIs can sometimes show nerve abnormalities, but MR neurography imaging is more sensitive, since it is specially tailored to image nerves. MR neurography uses advanced techniques to depict small nerves that may not be visualized on standard MRI exams. MR neurography is often used in conjunction with other examinations, including a physical exam, ultrasound, and electrodiagnostic testing, which includes electromyography (EMG).
MR neurography also provides visual clues about whether the muscles that an injured nerve supplies have atrophied or lost function as a result of the nerve damage.
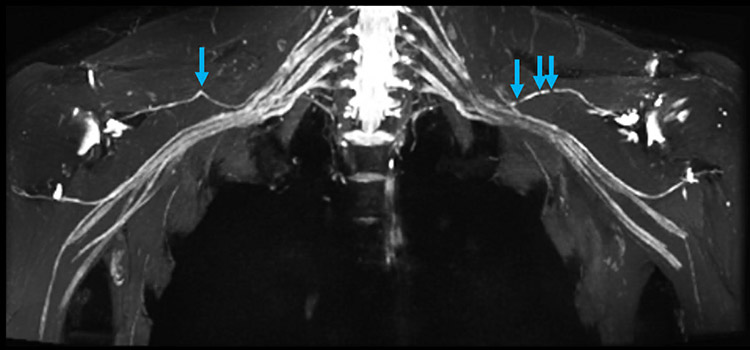
MR neurography of the bilateral brachial plexi in a patient with Parsonage-Turner syndrome demonstrates constrictions (blue arrows) of both suprascapular nerves.
Who should get MR neurography?
MR neurography can be performed on almost anyone with a suspected nerve injury. Symptoms of nerve damage may include pain, numbness, tingling, and muscle weakness. MR neurography can be performed as early as several hours or days following nerve injury. This has an advantage over electrodiagnostic studies, and in particular, electromyography (EMG), which usually requires at least a two- to three-week waiting period before being sensitive to damage. MR neurography can be used to diagnose many traumatic and atraumatic conditions that cause nerve compression, entrapment, or disruption:
- brachial plexus injury or lumbosacral plexopathy
- traumatic nerve injury
- Parsonage-Turner syndrome (PTS), also known as neuralgic amyotrophy
- anterior and posterior interosseous neuropathy
- spinal accessory neuropathy
- thoracic outlet syndrome
- sciatica and piriformis syndrome
- idiopathic neuropathy
- nerve entrapment, including:
- carpal tunnel syndrome (median nerve)
- cubital tunnel syndrome (ulnar nerve)
- tarsal tunnel syndrome (tibial/plantar nerves)
- meralgia paresthetica (lateral femoral cutaneous nerve)
- drop foot
- nerve injury around metallic hardware
- peripheral nerve sheath tumors (schwannoma and neurofibroma)
- pudendal neuralgia
- Charcot-Marie-Tooth disease
- chronic inflammatory demyelinating polyneuropathy (CIDP)
- multifocal motor neuropathy/MADSAM
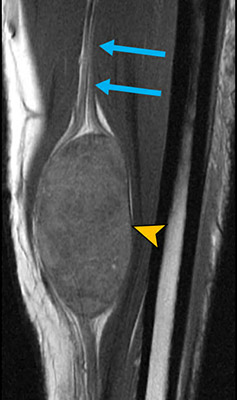
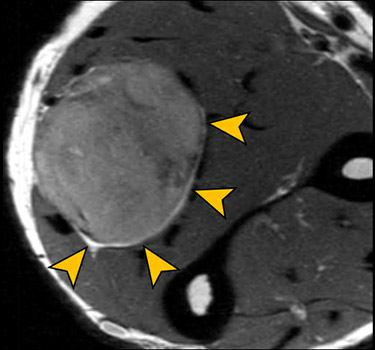
MR neurography showing a tumor (yellow arrowheads) arising from the ulnar nerve (blue arrows) in the forearm.
How does MR neurography work?
In many respects, MR neurography works similarly to standard MRI. It uses strong magnetic fields and radio waves to generate images. The thinly sliced, high-resolution images are designed specifically to enhance the appearance of nerves and muscle, rather than the bones, ligaments, and tendons depicted by more conventional musculoskeletal imaging. Specialized “pulse sequences” can be applied to improve nerve visualization. For example, reducing the signal (brightness) of nearby blood vessels (“vascular suppression”) or fat (“fat suppression”) enhances the appearance of the nerves.
Multiple sequences are usually required to evaluate a single region of the body. A set of pulse sequences grouped together is called the “imaging protocol.”
At HSS, all MR neurography exams are protocoled by an attending radiologist prior to the exam and monitored in real-time, in coordination with the performing technologist, to adjust the protocol as needed.
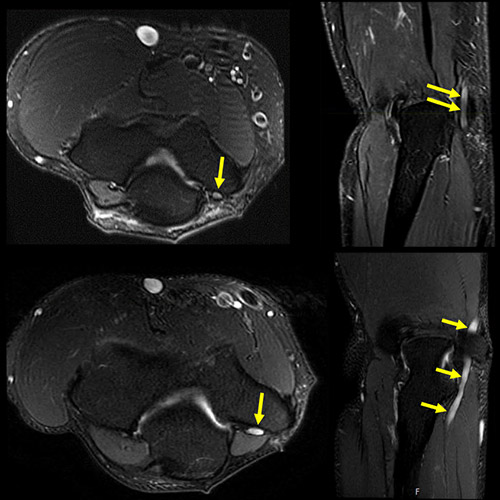
MR neurography images of a healthy ulnar nerve (top row) and an entrapped ulnar nerve in cubital tunnel syndrome (bottom row). The abnormal signal hyperintensity (brightness) of the nerve indicates neuropathy, with the nerve enlarged as it courses through the cubital tunnel at the elbow.
Is contrast used for MR neurography?
Some MR neurography exams use intravenous (IV) contrast to evaluate abnormalities or help differentiate nerves from surrounding structures. The contrast agent used in MR neurography exams is the same gadolinium-based contrast agent that is used for conventional MRI. Alternative contrast agents being investigated in our Magnetic Resonance Imaging Lab at Hospital for Special Surgery are sometimes given to patients who choose to participate in our ongoing research.
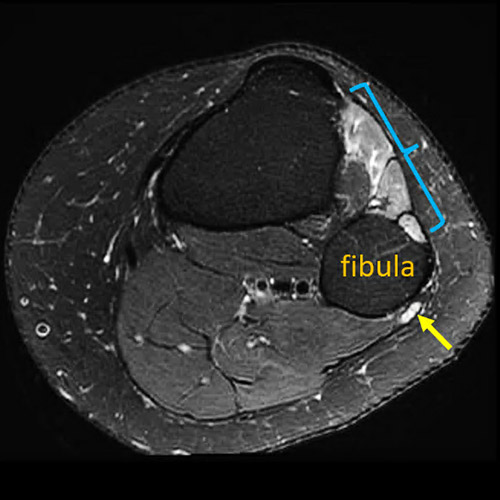
MR neurography showing spontaneous foot drop (denervation of lower leg muscles, highlighted by the blue bracket) due to neuropathy of the common peroneal nerve (yellow arrow)
as it courses around the fibula at the knee.
How long is an MR neurography exam?
The duration of an MR neurography exam varies with the area being imaged and other factors. Generally, a single exam lasts 45 to 60 minutes, but may be longer or shorter depending on individual circumstances.
What should I do to prepare for an MR neurography exam?
Preparing for an MR neurography exam is the same as preparing for a conventional MRI. There are no food or drink restrictions. You may take your medications as usual unless instructed otherwise.
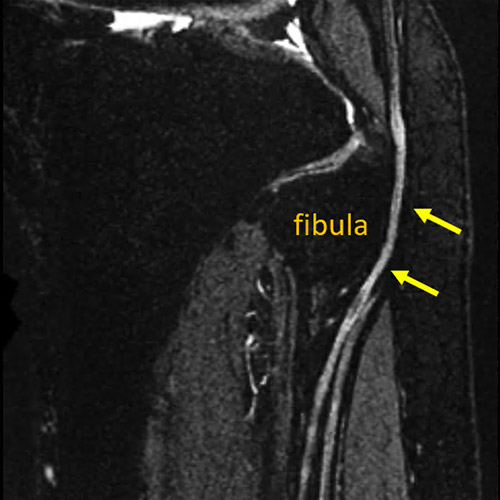
MR neurography shows abnormal signal intensity of the common peroneal nerve (yellow arrows) as it courses around the fibula at the knee.
Is MR neurography safe?
MR neurography is a very safe and well-tolerated exam. Like MRI, MR neurography does not involve the use of ionizing radiation as do traditional X-rays or CT scans.
Is MR neurography painful?
Patients will not experience any pain, but those with claustrophobia or aversion to loud noises may speak with their doctor ahead of time about possible modifications as well as with the technologist at the time of examination.
Can I have MR neurography if I have a medical implant?
Patients with hip, knee, shoulder or other joint replacements can usually undergo MR neurography. Patients who have certain medical devices or prostheses may not be able to have this type of imaging, or the procedure may need to be modified. Please let our team know if you have any metallic or electronic implants in your body.
What happens with my MR neurography results?
The radiologist will generate a written report, which will be made available to your referring physician within 24 to 48 hours of the exam. A copy of your report can be obtained through your MyHSS account typically within 24 hours of exam completion.
If your physician is at HSS, the images will be available immediately following the exam. Your physician will review the MR neurography test results with you and can correlate imaging results with clinical findings.
If your physician is an outside referring provider, a copy of your report will be faxed or mailed, free of charge, to that office. A disc containing the images will also be sent via FedEx. Physicians not on staff at HSS can request Portal Account access to images and reports associated with patients referred to HSS for imaging services. Additional copies of the images can also be obtained on a CD by contacting the file room at 212.606.1135.
MR neurography research at HSS
Our Magnetic Resonance Imaging (MRI) Lab is constantly working to improve techniques in MR neurography to diagnose and help manage an even wider range of clinical conditions. Current areas of investigation include:
- high-resolution techniques for peripheral nerve visualization
- imaging biomarkers of Parsonage-Turner syndrome (neuralgic amyotrophy)
- techniques, including diffusion MRI, to quantify the degree of nerve and muscle injury
- MRI coil development for spine and peripheral nerve imaging
- MRI nerve atlas development
Additional resources
- Patient webinar: Understanding Parsonage-Turner syndrome, Darryl Sneag, MD
- Webinar: MR Neurography of the Brachial Plexus, Darryl Sneag, MD
- GE Healthcare: AIR™ Recon DL, Darryl Sneag, MD
- Magnetic Resonance Neurography: Current Practice and Future Directions, Darryl Sneag, MD
- Society of Skeletal Radiology: Magnetic Resonance (MR) Neurography, Darryl Sneag, MD
- HSS MRI Lab Nerve Atlas Development
Schedule an
MR neurography
appointment
Call 212.774.7296
Updated: 4/17/2023
Authors
Director, MR Neurography and Director, MRI Research, Hospital for Special Surgery
Attending Radiologist, Hospital for Special Surgery
Associate Scientist, MRI Lab, Hospital For Special Surgery
Associate Professor of Biomedical Imaging in Orthopaedic Surgery, Weill Cornell Medical College

Related articles
References
- Brogan DM, Osei DA, Colorado BS, Sneag DB, Van Voorhis A, Dy CJ. Team Approach: Management of Brachial Plexus Injuries. JBJS Rev. 2022 Apr 15;10(4). doi: 10.2106/JBJS.RVW.21.00222. PMID: 35427254.
- Daniels SP, Feinberg JH, Carrino JA, Behzadi AH, Sneag DB. MRI of Foot Drop: How We Do It. Radiology. 2018;289(1):9-24. doi:10.1148/radiol.2018172634.
- Krishnan, K. R., Wolfe, S. W., Feinberg, J. H., Nwawka, O. K. & Sneag, D. B. Imaging and treatment of phrenic nerve hourglass‐like constrictions in neuralgic amyotrophy. Muscle Nerve 62, E81–E82 (2020).
- Motovilova, E. et al. Stretchable self-tuning MRI receive coils based on liquid metal technology (LiquiTune). Sci Rep-uk 11, 16228 (2021).
- Queler SC, Tan ET, Geannette C, Prince M, Sneag DB. Ferumoxytol-enhanced vascular suppression in magnetic resonance neurography. Skeletal Radiol. 2021 Nov;50(11):2255-2266. doi: 10.1007/s00256-021-03804-w. Epub 2021 May 7. PMID: 33961070.
- Queler, S. C., Towbin, A. J., Milani, C., Whang, J. & Sneag, D. B. Parsonage-Turner Syndrome Following COVID-19 Vaccination: MR Neurography. Radiology 211374 (2021) doi:10.1148/radiol.2021211374.
- Sneag, D. B. et al. Post-Contrast 3D Inversion Recovery Magnetic Resonance Neurography for Evaluation of Branch Nerves of the Brachial Plexus. Eur J Radiol 132, 109304 (2020).
- Sneag DB, Queler S. Technological Advancements in Magnetic Resonance Neurography. Curr Neurol Neurosci Rep. 2019;19(10):75. Published 2019 Aug 24. doi:10.1007/s11910-019-0996-x.
- Sneag, D. B., Zochowski, K. C. & Tan, E. T. MR Neurography of Peripheral Nerve Injury in the Presence of Orthopedic Hardware: Technical Considerations. Radiology 300, 246–259 (2021).
- Tan, E. T. et al. Quantitative MRI Differentiates Electromyography Severity Grades of Denervated Muscle in Neuropathy of the Brachial Plexus. J Magn Reson Imaging (2022) doi:10.1002/jmri.28125.
- Tan, E. T., Zochowski, K. C. & Sneag, D. B. Diffusion MRI fiber diameter for muscle denervation assessment. Quantitative Imaging Medicine Surg 12, 80–94 (2022).
- Zochowski, K. C. et al. Improvement of peripheral nerve visualization using a deep learning-based MR reconstruction algorithm. Magn Reson Imaging 85, 186–192 (2022).
- Zochowski KC, Tan ET, Argentieri EC, Lin B, Burge AJ, Queler SC, Lebel RM, Sneag DB. Improvement of peripheral nerve visualization using a deep learning-based MR reconstruction algorithm. Magn Reson Imaging. 2022 Jan;85:186-192. doi: 10.1016/j.mri.2021.10.038. Epub 2021 Oct 29. PMID: 34715288.



