Shoulder Labrum Tears: An Overview
Tears to the specialized cartilage tissue in the shoulder known as the labrum can cause pain and instability in the shoulder.
What is the labrum of the shoulder?
The labrum is a cup-shaped rim of cartilage that lines and reinforces the ball-and-socket joint of the shoulder. The shoulder joint is composed of the glenoid (the shallow shoulder "socket") and the head of the upper arm bone known as the humerus (the "ball"). The labrum is the attachment site for the shoulder ligaments and supports the ball-and-socket joint as well as the rotator cuff tendons and muscles. It contributes to shoulder stability and, when torn, can lead to partial or complete shoulder dislocation.
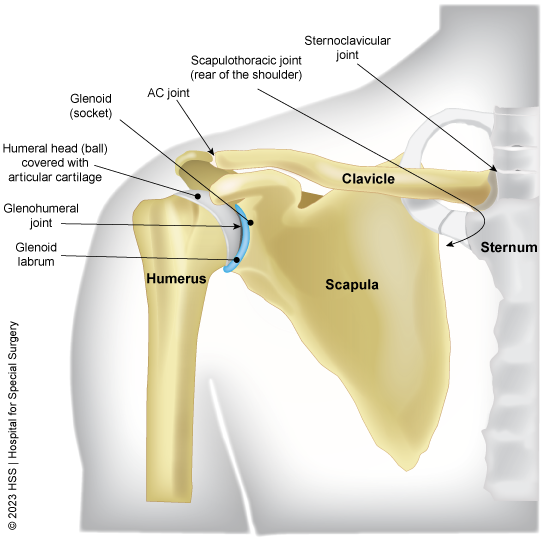
Illustration of the shoulder joint with the labrum shown in blue.
What does a torn shoulder labrum feel like?
The most common symptoms of a shoulder labrum tear are shoulder pain, instability and, in some cases, a feeling of grinding, locking or catching while moving the shoulder. These symptoms may vary depending on the type of labral tear a person has.
Among baseball players, pain is frequently felt when throwing, particularly between cocking and releasing the ball, and it may expand to the front of the shoulder during these movements. This soreness is frequently associated with biceps-related difficulties, such as releasing the ball and following through.
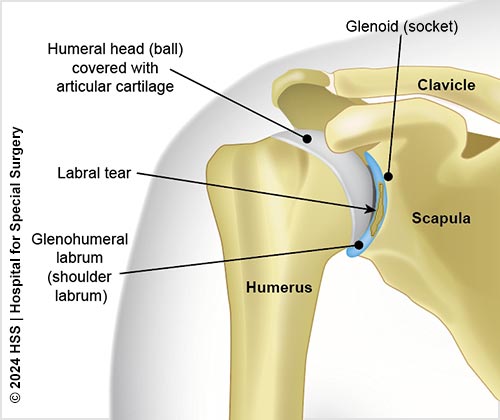
Illustration of the shoulder joint with a labral tear.
Patients often note that pain increases during activities that place strain on the shoulder, such as carrying large objects, pushing, throwing, or doing overhead tasks such as serving in tennis. Depending on the severity, they may have additional symptoms such as clicking, locking, snapping, grinding, or a sense that their shoulder is unstable.
What are the different types of shoulder labral tears?
The two most common types of labral injuries are the SLAP tear and Bankart tear. Both types of tears are usually accompanied by aching pain and difficulty performing normal shoulder movements.
SLAP tears
SLAP stands for "superior labrum from anterior to posterior." This type of tear occurs at the front of the upper arm where the biceps tendon connects to the shoulder. Athletes most prone to this injury include baseball pitchers, volleyball, and lacrosse players who engage in high-energy, quick-snap motions over the top of the shoulder which test the structures in the shoulder. This is why the term “overhead athletes” is often used when describing labral pathology. Patients with SLAP tears may experience pain at the front of the shoulder near the biceps tendon.
Bankart tears
Bankart tears typically occur in younger patients who have dislocated their shoulder. When the shoulder joint ball slips out of the socket, the joint capsule (fibrous tissues that surround and protect the joint) can pull on the lower portion of the labrum and tear it. This in turn creates instability because the breached labrum makes it easier for the shoulder to dislocate again. A dislocation where the head of the humerus shifts toward the front of the body, it leads to what is called "anterior instability." When the ball slips toward the back of the body, it leads to "posterior instability." Anterior instability is more common than posterior instability.
With Bankart tears, patients may feel apprehension that the shoulder may slip out of place or dislocate in certain positions.
Can labral tears of the shoulder be prevented?
Unfortunately, labral tears are hard to prevent, especially in athletes, because the force of the overhead motion contributes to the injury. Although athletes are most prone to labral tears, people who experience a traumatic event – such as falling down a flight of stairs – are also at risk. This is especially the case in older adults, because our cartilage becomes more brittle with age. (Find an HSS doctor who diagnoses and treats shoulder labral tears.)
Can a torn shoulder labrum tear heal on its own without surgery?
In some cases, the labrum can heal with rest and physical therapy, depending on the severity of the tear. Surgeons should try to be as conservative as possible when treating a torn shoulder labrum. Surgeons will start with a physical exam of the shoulder and an X-ray followed by an MRI if necessary to determine the severity of the injury and the appropriate treatment.
Torn labrum shoulder recovery without surgery
When surgery is not indicated, SLAP tears are usually treated with rest, anti-inflammatory medications and, in some cases, an in-office cortisone shot. This is followed by gradual stretching of the shoulder, initially with a physical therapist, for six weeks to two months. When appropriate, a platelet-rich-plasma (PRP) injection is a newer treatment that has promising results.
If the injury is a minor Bankart tear with a dislocation, the physician (or even a team coach or patient themselves) can usually pop the shoulder back into place – a process called reduction – and then follow up with physical therapy to strengthen the muscles.
When do you need surgery for a torn shoulder labrum?
Surgery may be required if the tear gets worse or does not improve after physical therapy. If physical therapy fails and the athlete still can’t complete overhead motions, or the shoulder continues to dislocate, surgical treatment might be required to reattach the torn ligaments and labrum to the bone. Arthroscopic procedures, in which the doctor operates through a small incision, are usually preferred because they are less invasive than open surgery.
In general, nonsurgical treatment is usually most appropriate for older patients who do not engage in regular physical activity, while younger athletes who regularly participate in higher impact sports can expect recurrence and may want to consider arthroscopic surgery.
(Find a shoulder surgeon at HSS.)
What is the recovery time for shoulder labrum repair surgery?
Patients who undergo arthroscopic repair can expect shorter recovery times and less pain. Those undergoing open surgery should expect more pain, longer recovery, and in some cases incomplete shoulder rotation. Athletes may require six months to one year for full recovery, with overhead throwing athletes taking the longest.
Regardless of which type of surgery is performed, almost all athletes are advised to wear a sling for the first four weeks after surgery to protect the shoulder as it heals. If fixed properly, most athletes should be able to return to at least 80% of their pre-injury level of play.
Updated: 9/12/2024
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Clinical Orthopedic Surgery, Weill Cornell Medical College
Related articles
Shoulder Labrum Tear Success Stories
References
- Eichinger JK, Li X, Cohen SB, Baker CL 3rd, Kelly JD, Dines JS, Tompkins M, Angeline M, Fealy S, Kibler WB. American Shoulder and Elbow Surgeons SLAP/Biceps Anchor Study Group evidence review: pathoanatomy and diagnosis in clinically significant labral injuries. J Shoulder Elbow Surg. 2023 May;32(5):e179-e190. doi: 10.1016/j.jse.2022.12.015. Epub 2023 Jan 19. PMID: 36681106. https://pubmed.ncbi.nlm.nih.gov/36681106/
- Zhang JY, Fabricant PD, Ishmael CR, Wang JC, Petrigliano FA, Jones KJ. Utilization of Platelet-Rich Plasma for Musculoskeletal Injuries: An Analysis of Current Treatment Trends in the United States. Orthop J Sports Med. 2016 Dec 21;4(12):2325967116676241. doi: 10.1177/2325967116676241. PMID: 28210648; PMCID: PMC5302101. https://pubmed.ncbi.nlm.nih.gov/28210648/



