Lumbar and Cervical Spondylosis: Symptoms and Treatments
Spondylosis is a nearly universal condition in those who reach advanced age, but it can also affect younger people. While some people experience no symptoms, others may feel stiffness and/or pain in the neck, shoulders or between the shoulder blades.
What is spondylosis?
Spondylosis is another word for osteoarthritis of the spine, a condition that usually develops with age, and is the result of normal “wear and tear” on both the soft structures and bones that make up the spine.
Although any part of the spine may be affected, spondylosis is more frequently seen in the spine’s highest and lowest sections – the cervical (neck) and lumbar (low back) areas, respectively. The condition is less commonly found in the thoracic spine (middle portion), possibly because the rib cage serves to stabilize this area and make it less subject to the effects of wear and tear over time.
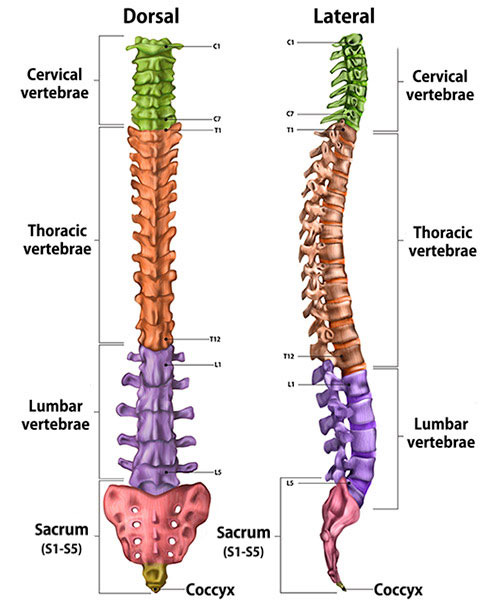
Illustration of cross-section of spine, dorsal (back to front) and lateral (side) views, showing its vertebral sections.
What are the symptoms of spondylosis?
People with spondylosis experience may or may not experience pain or, indeed, any symptoms at all. Those who have no symptoms may become aware of the condition only when they are being assessed for another medical issue that calls for imaging of the spine with an X-ray, MRI, or CT scan. When symptoms are present, they vary depending on the area where the condition develops and the structures that are affected, but they can include pain or limited range of motion.
Individuals with spondylosis who are otherwise without pain may experience crepitus, a feeling or sound of crunching in the spine, along with a limited range of motion. This usually is not concerning for nerve or spinal cord damage.
What are the symptoms of cervical spondylosis?
Neck pain and/or stiffness are common symptoms. In cases where spondylotic changes to the spine put pressure on adjacent nerves, patients may experience pain, numbness or tingling that extends down the arm, with or without symptoms in the neck itself. This type of nerve pain, which results from compression or inflammation of the nerve the cervical spine is known as cervical radiculopathy. Severe cases may also cause compression the spinal cord which may manifest as weakness or impaired motor function in the arms or hands, or other symptoms in a condition called cervical myelopathy.
What are the symptoms of lumbar spondylosis?
Low back pain, leg pain and/or other signs of nerve compression are the most common symptoms. Pain or tingling symptoms that extend outward to the hip or down the leg can result from compression or inflammation of nerves, a condition referred to as lumbar radiculopathy. For example, a person may have pain in their knee and think it is injured, but later learn that this pain is caused by spondylosis that is compressing a nerve which extends down to the knee. Irritation of the sciatic nerve in particular, is quite common, and is commonly known as sciatica.
Is spondylosis serious?
Because spondylosis can affect people in many different ways, there is no single answer to this question. Many cases of spondylosis are effectively treated with physical therapy and pain relief measures. However, orthopedists advise seeking more immediate care if the following symptoms, which are associated with pressure on the nerves, are present:
- weakness, including foot drop (difficulty lifting the toes and forefoot off the floor)
- bladder or bowel dysfunction, especially incontinence
- changes in balance that cannot be attributed to other factors
- numbness either in a stripe-like pattern or involving the fingers
- severe pain, especially electrical or shock like pain
- pain in the arms and/or legs that has not responded after attempting other nonsurgical measures like physical therapy, oral pain medications and/or spinal injections
Are some people more likely to develop spondylosis than others?
Spondylosis is likely to affect most people to some degree as they age, as it is the natural result of years of the spine being subject to the forces of gravity. There may be a genetic component (an inherited tendency) to develop the condition, but research has not clearly established this link.
An association between traumatic injury to the spine and the development of spondylosis later in life has been established.
How is spondylosis different from spondylolisthesis?
Although the names sound similar, spondylolisthesis is a condition in which one of the vertebrae (the bones that make up the spine) has moved out of place – usually in a forward direction. While this is a distinct diagnosis, spondylolisthesis may occur as a result of spondylosis, which can cause other structures of the spine move out of their normal position.
Other conditions that may result from spondylosis include:
- spinal stenosis – a narrowing of the spinal canal
- degenerative scoliosis – a sideways curvature of the spine due to osteoarthritis
- degenerative disc disease – wear and tear of the disc space
How is spondylosis diagnosed?
A diagnosis of spondylosis is based primarily on information seen on images of the spine: Changes to the bones are most clearly seen on X-ray, while changes to the soft structures – including the disks that act as cushions between the vertebrae – are more clearly seen on MRI or CT scans.
Abnormalities that may be detected include bone spurs, which are small growths of extra bone, or bulging or herniated discs. Both of these findings can cause narrowing in the spinal canal and put pressure on adjacent nerves. It’s important to note that wear and tear on the spine may show up on imaging tests, without the individual experiencing any pain or discomfort.
To better understand the impact spondylosis may be having on a patient, the orthopedist may order X-rays to look at the skeleton in motion, for example when the spine and neck bend backward or forward.
What type of doctor treats spondylosis?
People should first consult their primary care physician for back and neck pain. Persistent pain or symptoms associated with pressure on the nerves, such as weakness, are best assessed by a physician who specializes in musculoskeletal medicine, such as a physiatrist (a doctor who practices physical and rehabilitative medicine), a pain management doctor or a spine surgeon.
Once a diagnosis has been made, the type of physician who may best treat a patient’s symptoms depends on individual case. For many people, a physiatrist and physical therapist can treat people nonsurgically. Some others may benefit from interventional procedures, such as injections or radiofrequency ablation. In cases where spondylosis-related anatomic changes require removal or release of tissue, a spine surgeon will become involved. In some cases, your doctor or surgeon may also refer the patient to see a neurologist for additional care. (Find a doctor at HSS who treats spondylosis.)
How is spondylosis treated?
Treatment for spondylosis depends on the specific set of symptoms and findings that a patient is found to have and the area of the spine that is affected. Initial measures almost always include physical therapy to strengthen the muscles that support the spine and, in some cases, epidural steroid injections to reduce inflammation and pain. Short courses of oral pain medication, like anti-inflammatories, may also be prescribed.
Although non-operative treatment won’t change the structural effects of spondylosis – the wear and tear on tissues and the pressure on the nerves – it can provide relief while the nerve adapts to these changes in the spine anatomy. In many cases, this allows the symptoms to decrease without surgery.
What is the surgery for spondylosis?
If a person continues to have pain and debility from spondylosis after conservative measures are tried, surgical treatment may be recommended. The specific procedure needed depends on the abnormalities present in the spine, but it will generally involve addressing the area of the spine that is pressing on a nerve.
Some examples of minimally invasive surgical treatment for spondylosis include:
- removal of a bone spur in cervical spondylosis
- placement of spacers to recreate space lost by disc wear, allowing nerves to be free of compression
- removal of soft tissues that can become thickened in spondylosis that press on nerves
In some cases, a patient with spondylosis will require more extensive surgery to remove more a portion of the spine that is causing pain, and a fusion of the vertebrae, a surgery that stabilizes the bone. Anterior cervical discectomy with fusion (ACDF surgery) is one such procedure in the neck. For low back pain or other problems associated with lumbar spondylosis, a lumbar laminectomy, with or without fusion, or various other types of lumbar fusion surgery may be appropriate.
What is the recovery time for spondylosis surgery?
Recovery time varies depending on the nature of the surgery, with minimally invasive procedures permitting a more rapid return to daily activities. Many patients will complete a course of physical therapy beginning at six weeks after their operation. Keeping the supporting muscles flexible and strong and maintaining a healthy weight are the best way to prevent further problems in the spine.
Patients are also advised to assess and adjust ergonomic conditions that may have exacerbated their pain, for example raising a computer monitor to eye level to eliminate the tendency to hunch forward while doing office work.
Are there any dietary supplements that can help treat or prevent spondylosis?
There is no evidence at this time that any particular diet or supplement will help with spondylosis. It’s always a good idea to follow a healthy diet and to use supplements with caution, as these products are not regulated by the US Food and Drug Administration (FDA).
Updated: 4/17/2023
Authors
Sariah Khormaee, MD, PhD on behalf of HSS Spine
