Lupus and Heart Conditions – Top 10 Series
Many lupus patients experience serious heart problems, ranging from heart valve disease to heart attacks, as a result of their disease activity.

The following questions may help you better understand the different ways that lupus can affect your cardiac (heart) health. However, you should always speak with your doctor about symptoms and management of your disease.
- What is lupus?
- What is the structure (anatomy) of the heart?
- How common are heart complications in lupus patients?
- What are the different types of heart complications associated with lupus?
- Why is there increased risk of coronary heart disease in lupus?
- What are the symptoms of heart conditions in lupus patients?
- How are heart complications related to lupus diagnosed?
- How do you treat heart problems in lupus patients?
- What role do antiphospholipid antibodies play in lupus-related heart conditions?
- How can heart problems in lupus patients be prevented?
1. What is lupus?
Systemic lupus erythematosus (SLE or lupus) is a chronic, inflammatory autoimmune disease. In a person with lupus, persistent lupus-specific autoantibodies (antibodies that attack healthy proteins your body forms naturally) that are present in the blood cause organ inflammation and damage. Commonly affected organs in lupus patients are skin, joints, kidneys and blood cells. However, in some patients, lupus can also lead to heart conditions, some of which can be life-threatening.
2. What is the structure (anatomy) of the heart?
The heart has four chambers. The upper two chambers are called the left atrium and right atrium, and the lower two are called the left and right ventricles. These chambers are enclosed in a protective sac called the pericardium. Four valves regulate blood flow through the heart:
- The tricuspid valve regulates blood flow between the right atrium and right ventricle.
- The pulmonary valve controls blood flow from the right ventricle into the pulmonary arteries, which carry blood to the lungs to pick up oxygen.
- The mitral valve regulates blood flow between the left atrium and the left ventricle.
- The aortic valve controls the flow of the oxygen-rich blood from the left ventricle to the aorta, which is the main artery in the human body. Originating from the left ventricle, it distributes oxygenated blood to all parts of the body through the systemic circulation.
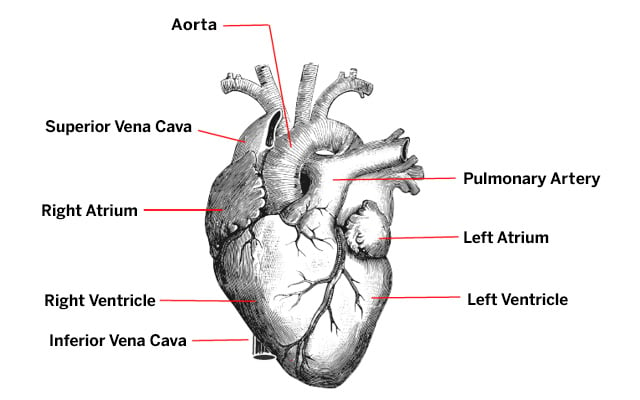
Image from Physiology for Young People: Adapted to Intermediate Classes and Common Schools. New York: American Book Co, 1888, p. 95.
- The heart wall is composed of muscular tissue, which is made up of three layers: epicardium outside, myocardium in the middle and endocardium inside. Blood vessels called coronary arteries provide blood flow to the heart.
- The inferior vena cava and superior vena cava are two large veins that return deoxygenated blood from the body back into the right atrium of the heart. Both empty into the right atrium. The inferior vena cava returns blood from the lower part of the body. The superior vena cava returns blood from head and the arms.
- Pulmonary arteries carry deoxygenated blood from the right side of the heart to the lungs. Pulmonary veins carry the oxygenated blood from the lungs to the left ventricle.
3. How common are heart complications in lupus patients?
About 50% of lupus patients experience heart complications as a result of their disease. For example:
- 20% to 40% of patients develop pericarditis or pericardial effusion (defined below).
- 10% to 15% of patients develop symptomatic myocarditis (defined below).
- The risk that a lupus patient will develop coronary heart disease is significantly higher than that of the general population.
4. What are the different types of heart complications associated with lupus?
Heart problems commonly associated with lupus include: pericarditis or pericardial effusion, valve abnormalities, myocarditis, rhythm disorders (arrhythmias), and accelerated atherosclerosis.
Pericarditis or pericardial effusion: This is the most common cardiac manifestation of lupus. Pericarditis means there is inflammation in the pericardium. Filling of the pericardium with inflammatory fluid is called “pericardial effusion.” If pericardial effusion is large or if it has accumulated rapidly, the fluid may compress the heart, causing cardiac tamponade, which may diminish the heart’s ability to contract. The pericardial fluid can also become infected by bacteria, causing infectious pericarditis.
Valve abnormalities: This is the accumulation of inflammatory cells within the valve tissue can cause thickening or nodules (bumps) on those valves. This condition is known as Libman-Sacks endocarditis (a noninfectious inflammation of the endocardium), which can cause narrowing of or leakage through the valves. These lesions can occur in any of the valves but are more commonly seen in the mitral and aortic valves. Disturbance in the blood flow can cause formation of blood clots (thrombosis) or vegetations (abnormal growths) on the valves. Fragments of these vegetations may emboli (travel in the arterial system) to the other organs. If the clot reaches the brain it can cause a mild or severe stroke. The heart valves can be infected by bacteria or fungi in 1% to 2% of the patients with valve disease. This condition is called infective endocarditis. On rare occasions, this complication can lead to a generalized infection in the body.
Myocarditis: This is the inflammation of the muscular tissue, the myocardium, of the heart. Myocarditis may cause impairment in the contractile function of the heart, making the heart get larger in size, and unable to pump blood. Other risk factors, such as hypertension (high blood pressure), kidney failure and medication toxicity (drug poisoning) can also contribute to the development of myocarditis.
Rhythm disorders (arrhythmias): These disorders cause the heart to beat too fast, too slow and/or irregularly, can also occur due to myocardial complications (for example, myocarditis). In rare occasions, myocardial problems can lead to severe arrhythmias and heart failure.
Accelerated atherosclerosis: Lupus patients have increased risk for atherosclerosis. Early and accelerated rate of atherosclerosis in lupus is not fully explained by the traditional risk factors for atherosclerosis (mainly the Framingham risk factors). Lupus-related factors including inflammatory mechanisms, disease duration, steroid therapy, and renal disease also contribute to enhanced atherosclerosis in lupus.
5. Why is there increased risk of coronary heart disease in lupus?
As discussed above, the risk of atherosclerosis and related coronary heart disease is higher among lupus patients. In fact, a younger woman (aged 35 to 44 years) with lupus is more than 50 times more likely to have a heart attack than women of similar age who don’t have lupus. This significant increase in the risk of heart disease in lupus patients is not explained by traditional risk factors for heart disease, such as age, gender, tobacco use, high blood pressure, or high cholesterol levels. Thus, inflammation related to lupus also plays a role in the increased risk of heart disease in lupus patients.
6. What are the symptoms of heart conditions in lupus patients?
Symptoms vary, depending on the individual conditions. They include rapid heartbeat associated with pericarditis or pericardial effusion, shortness of breath and heart palpitations for myocarditis, and abnormal heart rhythms. Additional symptoms may be present if a person with lupus experiences valve abnormalities or coronary heart disease.
Pericarditis or pericardial effusion: The most frequent symptoms are tachycardia (heart beating too rapidly), breathlessness, and chest pain increased by deep breathing, coughing, or swallowing. These symptoms tend to get worse when the patient is lying down.
Myocarditis: The common symptoms are fever, shortness of breath, and palpitations (feeling of your heart beating abnormally in the chest). Without treatment, this can lead to heart failure where heart muscle does not pump blood as well as it should leading to shortness of breath and swelling of the legs.
Rhythm abnormalities (arrhythmias): Heart rhythm abnormalities often do not cause any noticeable symptoms. However, these abnormalities can lead to palpitations (feeling of a “skipped” beat in the chest), fatigue, and fainting.
Valve abnormalities: These are also generally asymptomatic, but they can lead to a heart murmur, which your doctor can hear by listening to the heart with a stethoscope. If symptoms do arise, they can include shortness of breath, palpitations, cough and sometimes heart failure.
Coronary heart disease (also called coronary artery disease): Partial occlusion (blockage) of the coronary arteries can result in a dull chest pain on exertion, which rapidly disappears after a period of rest. A total occlusion can result in heart attack. Coronary artery disease can also cause cardiac dysfunction leading to heart failure which can present with swelling of the legs, shortness of breath, or decrease in urination.
7. How are heart complications related to lupus diagnosed?
A clinical examination by your doctor is the initial step. Then, most of the heart complications can be detected by one or more of the following:
- a simple electrocardiography (EKG), standard chest X-ray, echocardiography, Doppler investigation, or laboratory tests.
- if needed, excess pericardial fluid can be removed from the pericardial space for diagnosis, to rule out infection, by using a syringe (pericardiocentesis).
- as a further step, other tests may be necessary. These may include:
- cardiac exercise stress test.
- coronary angiogram.
- coronary computed tomography (CT scan).
- magnetic resonance imaging (MRI).
- biopsy of the heart muscle (endomyocardial biopsy).
8. How do you treat heart problems in lupus patients?
Most cardiac conditions in lupus patients can be treated with nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids. NSAIDs, such as ibuprofen and naproxen, decrease pain and inflammation. Corticosteroids, such as prednisone and methylprednisolone, are synthetic versions of a hormone naturally produced by the body and which helps suppress inflammation.
When lupus flare is severe, other immunosuppressive and/or immunomodulatory drugs can be used to suppress the disease activity. These may include:
- azathioprine
- mycophenolate mofetil
- belimumab
- cyclophosphamide
- intravenous immunoglobulin (IVIG)
In rare instances where symptoms of pericardial effusion are severe, it may be necessary to remove the excess pericardial fluid by inserting a needle into the chest and into the pericardial sac.
In case of heart failure, beta-blockers or angiotensin converting enzyme (ACE) inhibitors are recommended. In most severe cases, immediate admission to an intensive care unit (ICU) may be necessary to start mechanical heart assistance.
Heart valve problems generally do not require any treatment. Careful clinical monitoring and management of the lupus disease activity itself are adequate in most cases. In severe cases, however, valve surgery may be necessary. Surgical options include valve repair, replacement of the valve with a mechanical valve or a biologic valve.
In case of coronary artery disease, blood thinners (such as warfarin, aspirin) are used to prevent forming of blood clots in the damaged/inflamed coronary arteries. Systemic corticosteroids may be necessary to control the inflammation in the coronary arteries. Lifestyle modifications listed in the prevention section below are also recommended for all lupus patients.
Rhythm abnormalities can be treated with antiarrhythmic drugs, although in severe cases, invasive procedures such as implant of a pacemaker may be necessary.
9. What role do antiphospholipid antibodies play in lupus-related heart conditions?
About 30% to 40% of lupus patients produce antiphospholipid antibodies (aPL). These antibodies target the patient’s own blood vessels or clotting system proteins, causing blood clots in various organs in the body. Lupus patients with aPL have a higher risk of developing blood clots, valve disease, pulmonary hypertension, worse quality of life, and higher risk of organ damage, compared to the SLE patients without aPL. However, these antibodies do not increase the risk of heart inflammation (such as pericarditis and myocarditis). It is important to assess the aPL status of lupus patients and start blood thinners when needed.
10. How can heart problems in lupus patients be prevented?
Controlling lupus disease activity and preventing disease flares are the most helpful measures in preventing and managing the heart involvement in lupus.
Various lifestyle modifications are also recommended to all lupus patients to reduce the risk of coronary artery disease. Some of these measures include:
- Maintaining healthy diet habits with low intake of saturated fats and cholesterol
- Regular exercise
- Quitting smoking
- Maintaining ideal weight
- Decreased alcohol consumption
- Control of blood glucose levels to avoid diabetes
- Maintaining a normal blood pressure
References
- D’Cruz D, Khamashta M, Hughes G. Cardiovascular manifestations of systemic lupus erythematosus. In : Dubois' Lupus Erythematosus and Related Syndromes, 9th Edition. Eds : Wallace D, Hahn B. Philadelphia, Lippincott Williams & Wilkins. 2016; pp: 645-662.
- Yelnik CM, Richey M, Haiduc V et al. Cardiovascular Disease Prevention Counseling Program for Systemic Lupus Erythematosus Patients. Arthritis Care Res (Hoboken). 2017;69:1209-121.
- Esdaile JM, Abrahamowicz M, Grodzicky T et al. Traditional Framingham risk factors fail to fully account for accelerated atherosclerosis in systemic lupus erythematosus. Arthritis Rheum. 2001;44:2331-47.
- Giannelou M, Mavragani CP. Cardiovascular disease in systemic lupus erythematosus: A comprehensive update. J Autoimmun. 2017;82:1-12.
- Manzi S, Meilahn EN, Rairie JE et al. Age-specific incidence rates of myocardial infarction and angina in women with systemic lupus erythematosus: Comparison with the Framingham Study. Am J Epidemiol. 1997;145:408-15.
- Erkan D, Persad P, Rusli M. Top 10 Series: Lupus and Cardiovascular Disease (CVD) – Top Ten Points to Assess and Minimize Your CVD Risk. Accessed on February 23, 2019.
- Unlu O, Zuily S, ErkanD. The clinical significance of antiphospholipid antibodies in systemic lupus erythematosus. Eur J Rheumatol. 2016;3:75-84.
- Watad A, Tiosano S, Grysman N et al. The association between systemic lupus erythematosus and valvular heart disease: an extensive data analysis. Eur J Clin Invest. 2017;47:366-371.

