
What is LLIF/XLIF surgery?
Lateral lumbar interbody fusion (LLIF) is a minimally invasive surgery that helps treat low back pain by removing a damaged spinal disc and fusing the pain-generating spinal segment (the two vertebrae above and below the disc space). Extreme lateral interbody fusion (XLIF) is a proprietary system for performing a particular type of LLIF and is occasionally used to describe the LLIF procedure. In both procedures, the spinal segment (meaning two adjacent vertebrae and the disc space in between them) is fused using either an interbody spacer (or "cage") alone (known as a “stand-alone-LLIFâ€) or with additional instrumentation (posterior screws and rods).
Unlike other surgeries that approach the spine from the back (posterior) or abdomen (anterior), LLIF involves accessing the spine from the side (lateral). When appropriate for a particular patient’s case, this approach may allow surgeons to avoid major muscles, reducing tissue damage, blood loss, hospital stay, and recovery time.
Anatomy of the lumbar spine
The lumbar portion of the spine contains the five spinal vertebrae (L1 to L5) of the lower back.
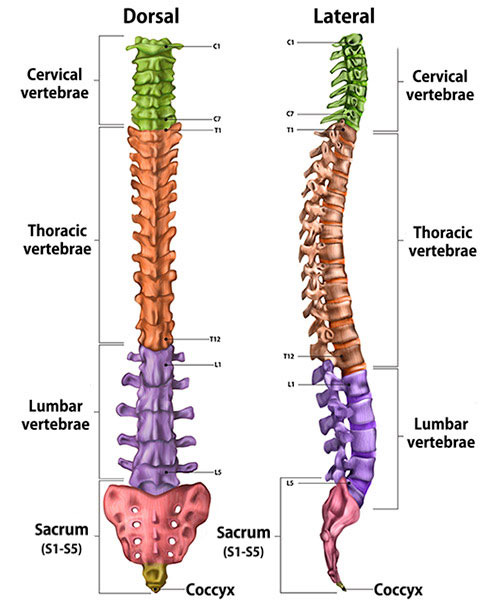
Illustration of cross-section of spine, dorsal (back to front) and lateral (side) views, showing its vertebral sections.
What is the difference between LLIF and XLIF?
XLIF (extreme lateral interbody fusion) is a trademarked name of Nuvasive, Inc. for their proprietary system of LLIF surgical tools and instrumentation, and it is occasionally used interchangeably to describe the LLIF procedure. Both terms generally describe the same type of surgery in which surgical tools access the spine through an incision on the side of the body.
What conditions does LLIF/XLIF surgery treat?
LLIF/XLIF surgery may be used to treat a range of conditions affecting the lumbar spine. These include degenerative disc disease (where the intervertebral discs lose elasticity and height, leading to pain and reduced mobility), spinal stenosis (a condition in which the spinal canal narrows and compresses nerves), spondylolisthesis (where one vertebra slips over another), and spinal deformity such as scoliosis or kyphosis (where the spine is misaligned).
This surgery may be performed in a single level (a one spinal segment) or multilevel (multiple segments), depending on the patient’s condition. (Find a surgeon at HSS who performs lumbar fusion surgeries.)
What are the advantages of LLIF/XLIF versus ALIF, PLIF or TLIF?
LLIF/XLIF may have several advantages stemming from its lateral (side) approach, which affects how the surgery is performed and the structures involved.
- Less invasive: LLIF is often performed through a smaller incision with less disruption of muscles and tissues, resulting in quicker recovery times, reduced hospital stays, and less postoperative pain.
- Reduced risk to major blood vessels and organs: The anterior approach (ALIF) poses a risk to major blood vessels and visceral organs. LLIF avoids this by taking a side approach.
- Shorter surgery time: Due to its minimally invasive nature, LLIF surgeries tend to be shorter, reducing the overall time under anesthesia and decreasing complication rates.
- Preserves back muscles: LLIF spares the posterior muscles, which helps maintain the spine’s natural stability and function.
- Improved posture correction: The lateral approach may allow for better correction of spinal alignment (lordosis) in cases of scoliosis or degenerative deformity than posterior approaches.
- Lower infection rates: Since LLIF avoids the large incisions and muscle dissections involved in PLIF and TLIF, the risk of infection may be lower.
What are some limitations of LLIF/XLIF surgery?
LLIF has some limitations and considerations, including its unsuitability for addressing issues at the L5-S1 level (where the lowest lumbar vertebrae meet the sacrum), because the iliac crest of the pelvic bone obstructs a lateral approach).
There is also a risk of nerve injury, particularly as the surgeon navigates through one of the low back muscles, though intra-operative neuromonitoring reduces this risk. For these reasons, it may not be appropriate for all patients or spinal conditions, depending on individual anatomy and pathology.
How is LLIF/XLIF spine surgery performed?
LLIF/XLIF is a minimally invasive spine surgery performed through a side approach. The patient is usually positioned on their side, and the surgeon makes a small incision to access the spine, avoiding major back muscles. Using real-time imaging, the surgeon removes the damaged disc and inserts a spacer or cage filled with bone graft material to restore disc height and relieve nerve pressure. This promotes fusion between the vertebrae, and sometimes additional hardware is added for stability.
The lateral approach reduces muscle damage, resulting in less pain and quicker recovery compared to traditional spinal surgeries.
Video: Animation of lateral lumbar interbody fusion
Stand-alone LLIF (spacer or cage without additional instrumentation) can be considered in cases where a patient requires spinal stabilization or correction but has a relatively straightforward condition that doesn’t require additional support from rods or screws. It's typically recommended for patients with degenerative disc disease, mild cases of spondylolisthesis, or spinal stenosis, where the main issue is disc degeneration or nerve compression without severe instability or deformity.
Stand-alone LLIF is ideal when the goal is to minimize muscle disruption and preserve motion in adjacent levels of the spine, offering quicker recovery and reduced surgical risks. It is also considered in patients who have minimal osteoporosis, whereas in patients who have more severe osteoporosis, the osteoporotic bone may require added posterior fixation support to ensure successful fusion. The decision to use stand-alone LLIF depends on the patient’s anatomy, the degree of spinal instability, and the surgeon’s assessment of whether extra hardware is necessary for optimal outcomes.
LLIF with instrumentation may be used if there is spinal instability or the surgeon assesses that extra hardware is necessary for optimal outcomes.
How long does LLIF/XLIF surgery take?
A lateral interbody fusion surgery, such as LLIF or XLIF, typically takes 1.5 to 3 hours to complete. The duration can vary depending on factors like the complexity of the case, the number of spinal levels being treated, the patient's anatomy, and whether additional hardware (such as screws or rods) is required for stabilization. The minimally invasive nature of the procedure helps keep surgery time relatively short compared to traditional open spinal fusion surgeries.
What is the recovery time for LLIF/XLIF?
The recovery time for XLIF and LLIF generally involves a hospital stay of 1 to 2 days, with most patients able to resume light activities within 1 to 2 weeks. Many can return to desk-based work within 4 to 6 weeks, while full recovery, including returning to more strenuous activities, may take 3 to 6 months. Participation in physical therapy and following the surgeon's post-operative instructions are essential for optimal recovery and healing. Regular follow-ups are also important to monitor progress and ensure proper fusion of the vertebrae.
How long does back pain last after LLIF surgery?
Back pain varies by individual. While some patients may find immediate relief, others might experience post-operative discomfort that lasts for several weeks to months. Typically, acute pain from the surgery decreases within 2 to 6 weeks, but lingering pain can persist for 3 to 6 months as the body heals and fuses the vertebrae.
How soon can you walk after LLIF surgery?
Most patients start walking within a few hours after surgery, often on the same day as the procedure. Walking is encouraged early in the recovery process to promote circulation, prevent blood clots, and aid in healing.
Do you need physical therapy after LLIF surgery?
Physical therapy is often recommended after surgery to aid in recovery and improve outcomes. Physical therapy typically begins shortly after the surgery, focusing on gentle movements and exercises to enhance mobility, strengthen the back and core muscles, and improve overall function.
What risks or complications can occur with LLIF/XLIF surgery?
LLIF/XLIF surgeries, while minimally invasive, carry some risks and potential complications. These may include nerve injury (particularly to the lumbar plexus, leading to weakness or numbness in the legs), vascular injury due to proximity to blood vessels, infection at the surgical site, and complications related to anesthesia.
Other risks include insufficient bone fusion (nonunion), which may require additional surgery, and the possibility of adjacent segment disease, where nearby vertebrae may become stressed over time. Patients are encouraged to discuss these risks with their surgeon to make an informed decision about the procedure.
What is the success rate for lateral lumbar interbody fusion?
The success rate for lateral lumbar interbody fusion (LLIF) and its variant, XLIF, generally ranges from 80% to 90%. Success is typically defined by significant pain relief, improvement in function, and achieving solid fusion of the vertebrae. Factors that influence the success of the surgery include the patient's overall health, the specific condition being treated, the presence of any other spinal issues, and adherence to post-operative rehabilitation and care.
Posted: 11/7/2024
Authors
Mihir Dekhne, MD
Orthopaedic Surgery Resident
Hospital for Special Surgery
Attending Orthopedic Surgeon, Hospital for Special Surgery
Research Director, Spine Service, Hospital for Special Surgery
Related articles
References
- Camino-Willhuber G, Tani S, Shue J, Zelenty WD, Sokunbi G, Lebl DR, Cammisa FP, Girardi FP, Hughes AP, Sama AA. Lumbar lateral interbody fusion: step-by-step surgical technique and clinical experience. J Spine Surg. 2023 Sep 22;9(3):294-305. doi: 10.21037/jss-23-54. Epub 2023 Sep 12. PMID: 37841793; PMCID: PMC10570643. https://pubmed.ncbi.nlm.nih.gov/37841793/
- Nolte MT, Gandhi SD, Nguyen AQ, Siyaji ZK, Piracha AZ, Khanna K, Rush AJ 3rd, Sheha ED, Phillips FM. Rates of Postoperative Complications and Approach-related Neurological Symptoms After L4-L5 Lateral Transpsoas Lumbar Interbody Fusion Compared With Upper Lumbar Levels. Clin Spine Surg. 2023 Aug 1;36(7):E294-E299. doi: 10.1097/BSD.0000000000001367. Epub 2022 Aug 10. PMID: 35945666.
https://pubmed.ncbi.nlm.nih.gov/35945666/ - Oezel L, Okano I, Hughes AP, Sarin M, Shue J, Sama AA, Cammisa FP, Girardi FP, Soffin EM. Longitudinal Trends of Patient Demographics and Morbidity of Different Approaches in Lumbar Interbody Fusion: An Analysis Using the American College of Surgeons National Surgical Quality Improvement Program Database. World Neurosurg. 2022 Aug;164:e183-e193. doi: 10.1016/j.wneu.2022.04.067. Epub 2022 Apr 25. PMID: 35472646.https://pubmed.ncbi.nlm.nih.gov/35472646/
- Salzmann SN, Fantini GA, Okano I, Sama AA., Hughes AP, Girardi FP. Mini-Open Access for Lateral Lumbar Interbody Fusion: Indications, Technique, and Outcomes. JBJS Essent Surg Tech. 2019 Nov 1;9(4):e37.1-10. doi: 10.2106/JBJS.ST.19.00013. PMID: 32051785; PMCID: PMC6974316. https://pubmed.ncbi.nlm.nih.gov/32051785/
- Shafi K, Lovecchio F, Song J, Qureshi S. Robotic-Assisted Single-Position Prone Lateral Lumbar Interbody Fusion: Indications, Techniques, and Outcomes. JBJS Essent Surg Tech. 2023 Nov 15;13(4):e22.00022. doi: 10.2106/JBJS.ST.22.00022. PMID: 38357472; PMCID: PMC10863943. https://pubmed.ncbi.nlm.nih.gov/38357472/
- Winebrake JP, Lovecchio F, Steinhaus M, Farmer J, Sama A. Wide Variability in Patient-Reported Outcomes Measures After Fusion for Lumbar Spinal Stenosis: A Systematic Review. Global Spine J. 2020 Apr;10(2):209-215. doi: 10.1177/2192568219832853. Epub 2019 Mar 4. PMID: 32206520; PMCID: PMC7076598. https://pubmed.ncbi.nlm.nih.gov/32206520/
