Lupus, Osteopenia and Osteoporosis – Top 10 Series
Top 10 Points Lupus Patients Should Be Aware of Regarding Osteopenia and Osteoporosis
- What is systemic lupus erythematosus?
- What is osteopenia and what is osteoporosis?
- How do you measure and define osteopenia and osteoporosis?
- What are the risk factors for osteopenia and osteoporosis in the general population?
- What are lupus-specific risk factors for osteopenia and osteoporosis?
- How common is osteopenia and osteoporosis in lupus patients?
- When should lupus patients be screened for osteoporosis?
- What is the recommendation to prevent osteoporosis in lupus patients?
- What are the treatment options for osteopenia and osteoporosis in lupus patients?
- What are the serious complications of osteoporosis?
1. What is systemic lupus erythematosus?
Systemic lupus erythematosus (SLE or “lupus”) is a chronic autoimmune disease that can affect most tissues and organs in the body. Lupus mostly affects women. Hormonal, environmental, and genetic factors contribute to the development of disease. There may be a wide variety of symptoms in lupus patients, however the most common symptoms are joint pain and swelling, a butterfly-like rash on the face, and kidney disease.
2. What is osteopenia and what is osteoporosis?
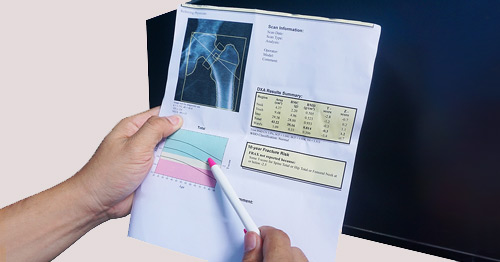
Osteopenia and osteoporosis are terms that refer to the bone mineral density (BMD) as measured by Dual X-ray Absorptiometry (DEXA). Bone mineral density is a surrogate for bone strength. Patients with osteopenia and osteoporosis are at increased risk of fractures due to decreased BMD (see next question for definitions).
3. How do you measure and define osteopenia and osteoporosis?
Bone mineral density can be measured with a special X-ray called Dual X-ray Absorptiometry (DEXA), a short, non-invasive, and painless test that uses very low-dose radiation. With the DEXA method, the bone mineral density (BMD) in different parts of the body can be measured. This usually includes the lumbar spine (lower back), hip and forearm. The results of the test are reported as:
- Z-score: BMD compared to individuals of the same age.
- T-score: BMD compared to a healthy 30-year-old (the age of one’s peak bone mass).
- The T-score is the recommended benchmark for postmenopausal women and men over age 50. The Z-score is recommended in children, premenopausal women and men under age 50.
- A T-score of 0 to -1.0 defines a normal bone mineral density.
- A T-score between -1.1 and -2.4 defines osteopenia.
- A T-score of -2.5 or greater defines osteoporosis.
4. What are the risk factors for osteopenia and osteoporosis in the general population?
On average, peak bone mineral density (BMD) is reached by the age of 30. After that, BMD starts to decline. There is a slow and steady decline for men, while women lose bone more rapidly around menopause. Some of the factors that contribute to BMD decline include:
Unchangeable factors
- age
- gender
- ethnicity
- genetic background
- family history of osteoporosis
Lifestyle-related factors
- lack of physical activity
- insufficient calcium and vitamin D intake
- immobilization
- smoking
- excessive use of alcohol
Chronic diseases
- chronic kidney diseases
- blood-cell-related diseases and cancers
- gastrointestinal diseases, such as celiac disease
- rheumatologic diseases such, as rheumatoid arthritis and lupus
- hormonal and endocrinologic diseases, such as diabetes mellitus, hyperparathyroidism and hyperthyroidism
Other
- pregnancy
- lactation
5. What are lupus-specific risk factors for osteopenia and osteoporosis?
Lupus-specific risk factors that contribute to osteopenia and osteoporosis include:
- Lupus disease activity: Inflammation disrupts bone remodeling, the process by which our bodies continually renew our bone tissue. It reduces new bone formation while increasing bone resorption (the breakdown of mature bone tissue). This results in a net bone loss.
- Low vitamin D levels resulting from decreased sun exposure, since people with lupus generally avoid sun exposure because of their sensitivity to sunlight.
- Lupus kidney disease, which decreases vitamin-D levels and increases levels of parathormone (also known as parathyroid hormone, this is a hormone that regulates calcium levels in the bloodstream; an increase of this hormone causes an increase in bone resorption.
- Lupus medications, such as corticosteroids.
6. How common is osteopenia and osteoporosis in lupus patients?
Osteoporosis is the most common metabolic bone disease worldwide, affecting more than 200 million people. This condition affects females four times more compared to males. The National Osteoporosis Foundation (NOF) reported that 10.2 million people in the United States over 50 years of age have osteoporosis, while 43.4 million have a low bone mineral density (osteopenia). In people over 50 years old, the frequency of low BMD is approximately 45%, and osteoporosis 15%.
Based on different studies and the age of the population studies, osteopenia in lupus patients is detected in between 25% to 75% of patients, and osteoporosis in anywhere from 2% to 68%.(Bultink IE.)
7. When should lupus patients be screened for osteoporosis?
In the general population, bone mineral density (BMD) screening is recommended for women at menopause and for men over the age of 70.
The risk of osteopenia and osteoporosis, and the need for BMD screening, should be assessed regularly in all lupus patients. Within six months of the starting corticosteroid therapy, BMD screening is recommended in lupus patients, and the test should be repeated every one to two years.
8. What is the recommendation to prevent osteoporosis in lupus patients?
In patients with lupus undergoing corticosteroid therapy at a dose of 5mg a day or more of prednisone equivalent for longer than three months, vitamin D replacement and calcium supplementation are recommended. It is also recommended to start vitamin D replacement at the time of the first diagnosis in patients with lupus nephritis. There are also general recommendations such as:
- regular exercise
- alcohol use in moderation
- smoking cessation
- sufficient calcium and vitamin d intake
- healthy weight as being underweight is associated with osteoporosis
9. What are the treatment options for osteopenia and osteoporosis in lupus patients?
The management of osteopenia is based on appropriate lifestyle change recommendations including:
- calcium supplementation for those with insufficient intake
- vitamin-D replacement to maintain the 25-OH-Vitamin D level above 30 ng/mL
- exercise (weightbearing exercises recommended, such as dancing, walking, and climbing stairs)
- maintaining a healthy diet containing calcium- and vitamin D-rich products
There are various medical treatments recommended for osteoporosis and patients should discuss the choice of medication with their physicians. The most commonly used medications are bisphosphonates, which reduce bone resorption. Some bisphosphonate medications are:
- alendronate (Fosamax®)
- risedronate (Actonel®, Atelvia®)
- İbandronate (Boniva®)
- zolendronic acid (Reclast®)
Other osteoporosis treatment options include:
- Rank-L inhibitor: Denosumab (Prolia®), which reduces bone resorption.
- Parathyroid hormone and parathyroid-related protein: Teriparatide (Forteo®) and Abaloparatide (Tymlos®), are known as anabolic agents and increase bone formations.
- Romosozumab (Evenity®), which increases bone formation and reduces bone resorption.
10. What are the serious complications of osteoporosis?
Osteoporosis is also known as a silent disease; however, fractures are the most important clinical complication, affecting 20% of men and 50% of women over 50 years of age. Lupus patients have five times increased risk of fracture compared to the general population.(Ramsey-Goldman R, et al.) Vertebral compression fracture is the most common osteoporosis-related fracture in the United States.
Vertebral fractures can result in:
- posture problems, kyphosis and chronic pain
- early satiety
- decrease in functional capacity and immobility
Hip fractures can result in:
- immobility, reduced independence, and increased hospitalization
- chronic pain, depression, and social isolation
- increased risk of mortality
Posted: 3/10/2023
Authors
Attending Physician, Hospital for Special Surgery
Director of Perioperative Services, Hospital for Special Surgery
Attending Rheumatologist, Hospital for Special Surgery
Professor of Medicine, Weill Cornell Medical College
Related articles
References
- Buyon JP, Petri MA, Kim MY, Kalunian KC, Grossman J, Hahn BH, et al. The effect of combined estrogen and progesterone hormone replacement therapy on disease activity in systemic lupus erythematosus: a randomized trial. Ann Intern Med. 2005;142(12 Pt 1):953-62.
- Grossman JM, Gordon R, Ranganath VK, Deal C, Caplan L, Chen W, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken). 2010;62(11):1515-26.
- Porter JL, Varacallo M. Osteoporosis. StatPearls. Treasure Island (FL)2022.
- Zucchi D, Elefante E, Calabresi E, Signorini V, Bortoluzzi A, Tani C. One year in review 2019: systemic lupus erythematosus. Clin Exp Rheumatol. 2019;37(5):715-22.
- Buckley L, Guyatt G, Fink HA, Cannon M, Grossman J, Hansen KE, et al. 2017 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis. Arthritis Care Res (Hoboken). 2017;69(8):1095-110.
- Almehed K, Forsblad d'Elia H, Kvist G, Ohlsson C, Carlsten H. Prevalence and risk factors of osteoporosis in female SLE patients-extended report. Rheumatology (Oxford). 2007;46(7):1185-90.
- Adami G, Fassio A, Rossini M, Caimmi C, Giollo A, Orsolini G, et al. Osteoporosis in Rheumatic Diseases. Int J Mol Sci. 2019;20(23).
- Bultink IE. Osteoporosis and fractures in systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2012;64(1):2-8.
- Medeiros MM, Silveira VA, Menezes AP, Carvalho RC. Risk factors for ovarian failure in patients with systemic lupus erythematosus. Braz J Med Biol Res. 2001;34(12):1561-8.
- Sheu A, Diamond T. Secondary osteoporosis. Aust Prescr. 2016;39(3):85-7.
- Mäkitie O, Zillikens MC. Early-Onset Osteoporosis. Calcif Tissue Int. 2022;110(5):546-61.
- American College of Rheumatology. 2022 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis (GIOP). Published online September 14, 2022. Accessed September 21, 2022.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-30.
- Sarafrazi N, Wambogo EA, Shepherd JA. Osteoporosis or Low Bone Mass in Older Adults: United States, 2017–2018. 2021.
- Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin D, Calcium. The National Academies Collection: Reports funded by National Institutes of Health. In: Ross AC, Taylor CL, Yaktine AL, Del Valle HB, editors. Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC)2011.
- Varacallo M, Seaman TJ, Jandu JS, Pizzutillo P. Osteopenia. StatPearls. Treasure Island (FL)2022.
- Yu JS, Krishna NG, Fox MG, Blankenbaker DG, Frick MA, Jawetz ST, et al. ACR Appropriateness Criteria® Osteoporosis and Bone Mineral Density: 2022 Update. J Am Coll Radiol. 2022;19(11s):S417-s32.
- Chou S, Grover A, LeBoff MS. New Osteoporotic/Vertebral Compression Fractures. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, et al., editors. Endotext. South Dartmouth (MA)2000.
- Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761-7.
- Ramsey-Goldman R, Dunn JE, Huang CF, Dunlop D, Rairie JE, Fitzgerald S, et al. Frequency of fractures in women with systemic lupus erythematosus: comparison with United States population data. Arthritis Rheum. 1999;42(5):882-90.



