Cervical Laminoplasty
Decompression neck surgery to remove pressure on the spinal cord and nerves caused by spinal stenosis
There are several forms of spinal decompression surgery that spine surgeons may perform to relieve pressure on the spinal cord and nerves in the neck. One such procedure is a cervical laminoplasty.
What is cervical laminoplasty surgery?
Cervical laminoplasty is a specialized procedure for relieving pressure on the spinal cord at the level of the neck (cervical spine). Laminoplasty differs from traditional spinal surgery in two important ways:
- No bone is removed during the procedure. Rather, bone is reshaped by the surgeon.
- The bones are not purposefully fused together, which preserves the natural motion of the spine.
There are several different methods for performing this procedure, but all rely on the same principle of expanding the spinal canal to make room for the spinal cord.
Spine anatomy and stenosis
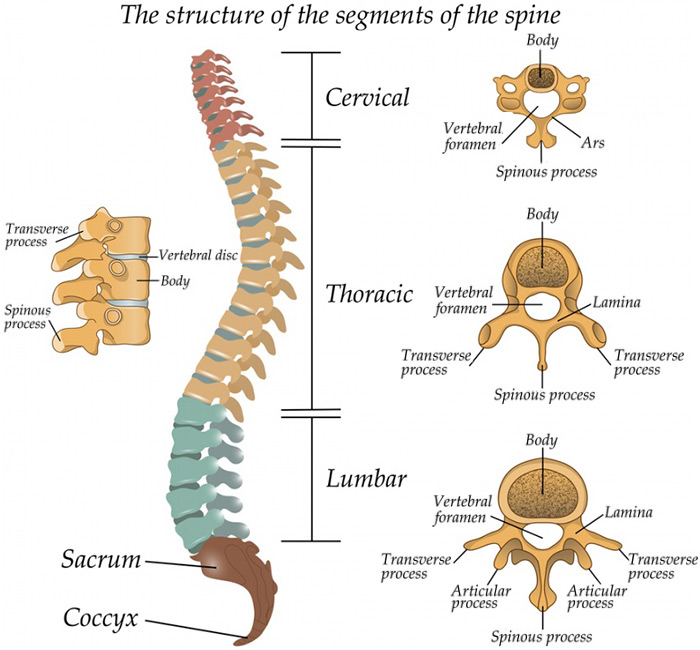
The human brain rests comfortably within the bony skull and it communicates with the rest of our body through the spinal cord and its nerves. The spinal cord extends from the base of the brain and enters the spinal canal – a protective space within our bony spine.
The spine is divided into three sections, named for their location and function:
- The cervical spine composes the body’s neck and allows body to turn the head in many directions.
- The thoracic spine supports the rib cage, protecting the heart, lungs, and large vessels.
- The lumbar spine connects the torso to the pelvis and allows the body to bend, flex, and twist around the torso.
In most cases, there is plenty of room within the bony spine for the spinal cord and nerve roots to exist comfortably and function normally. However, some processes, including everyday wear-and-tear, can cause narrowing of the spinal canal. At the level of the cervical spine, this narrowing can eventually get so bad that the spinal cord itself is compressed and unhealthy. Spine surgeons at HSS can use cervical laminoplasty to relieve this pressure while preserving the motion of the cervical spine. (Find a surgeon who does laminoplasty surgery.)
How does a surgeon perform a cervical laminoplasty?
There are many steps in performing a cervical laminoplasty, including appropriate anesthesia, positioning the patient, the procedure itself, and safely transferring the patient to the recovery room.
Cervical laminoplasty surgery requires the use of general anesthesia (where the patient is completely asleep and a breathing tube inserted to assist with breathing) to ensure that the patient is comfortable throughout the procedure. The anesthesiologist monitors the patient throughout the case to make sure that it proceeds safely. Once the patient is asleep and comfortable, the neuromonitoring team places electrodes in muscles along the patient’s legs and arms and in the scalp to keep track of the spinal cord and nerve root health during the procedure.
In order to access the back of the cervical spine, the patient’s head is secured using a specialized clamp or similar device and then laid prone (lying face down) on a well-padded bed. The patient’s arms are tucked comfortably along the side of their body during the procedure.
Once the area has been sterilized and draped, it is time to start the procedure. An incision is made in the center of the back of the neck along the spine. This incision is usually two to three inches long from just below the base of the skull to the base of the neck. The soft tissue and muscle are carefully dissected away from the bony spine, revealing the lamina.
Animation of a cervical laminoplasty
There are several techniques to perform the laminoplasty itself. One common technique turns the lamina into a “door on a hinge.” Using delicate tools, a small trough is cut on one side of the lamina, taking care to protect the spinal cord and roots. On the opposite side, an incomplete cut or scoring is performed. The bone is then “hinged” open along the incomplete cut. The door is held open and secured using plates and screws or bone graft. This “open door” technique expands the canal upwards of 30%. The soft tissue is then carefully replaced using absorbable suture up to the skin. A sterile bandage is applied and then the patient is carefully returned to their hospital bed, awakened from anesthesia, and transferred to the recovery area.
Who is a good candidate for cervical laminoplasty?
The goal of cervical laminoplasty is to increase room in the spinal canal while preserving the motion in the neck. This is most appropriate for patients who have some form of central spinal stenosis (narrowing of the spinal canal). The most common reasons for performing cervical laminoplasty include cervical stenosis, ossification of the posterior longitudinal ligament, and cervical spondylotic myelopathy.
Cervical stenosis is a broad diagnosis and can be caused by many processes, including arthritic changes of the spine, problems with blood vessels, tumors, etc. These processes result in a narrowing of the bony spine, which can cause compression of the spinal cord and its roots. This may cause patients to experience pain and changes in their sensation (for example a sense of “pins and needles” along a nerve). Cervical laminoplasty will restore space to the cord and roots.
Ossification of the posterior longitudinal ligament (or OPLL for short) is a hardening of connective tissue around the bony spine. This hard tissue expands and creates pressure on the spinal cord. Due to the technical difficulty of addressing this problem from the front (anterior) of the spine, through ACDF surgery, a laminoplasty or other surgery performed through the back (posterior) of the spine is preferred.
Cervical spondylotic myelopathy is a special condition that occurs due to spondylosis (arthritis of the spine). An arthritic spine produces bone spurs and other inflamed tissue which presses on the spinal cord so severely that the cord is not able to function properly. When the cord is unable to function properly, this is known as myelopathy. To prevent this condition from getting worse, a cervical laminoplasty can be performed.
A laminoplasty procedure may not be appropriate for some patients, and patients should discuss their treatment options with their surgeon. For example:
- One of the goals of laminoplasty, as mentioned before, is to preserve natural motion of the spine. In patients with advanced arthritis of the spine, there may not be much motion, if at all. The laminoplasty procedure cannot restore motion but only allows the spine to keep most of the motion it has currently.
- Similarly, the alignment of the cervical spine is important to consider prior to performing a laminoplasty. Some patients may have a deformity or poor alignment of their cervical spine which would cause a laminoplasty procedure to be unsuccessful, whereas a more traditional spine procedure would work much better.
What is a laminoplasty versus a laminectomy or laminotomy?
A laminoplasty will reshape a vertebral lamina, a laminectomy will remove the lamina, and a laminotomy will make a small opening in the lamina. These procedures can be used for different types of spinal diseases. Patients should discuss treatment options with their surgeons to learn more.
Medical jargon can seem very complex, but most words can be broken down into parts to better understand their meaning. When looking at the bony spine in cross-section, the “lamina” forms a “roof” over the spinal canal. The vertebral body forms the “floor” and the “pedicles” which connect the body to the lamina form the walls. The spinal cord and its roots pass through the protective space within this “house” analogy.
Viewed in cross-section, the complex anatomy of the bony spine and the spinal canal is clearer. This complex structure can be thought of as a house sitting on a foundation. In the diagram below, the bony spine is represented by the chimney, roof, and walls of the house connected at the foundation to the bony vertebral body. The spinal cord and nerve roots are protected within the walls of the house.
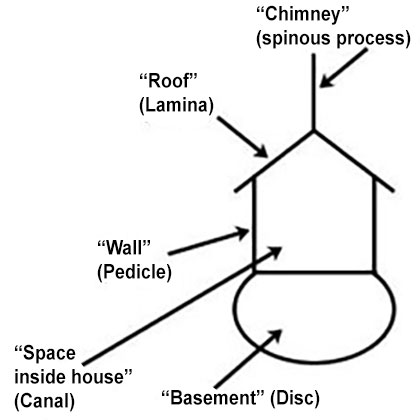
Diagram of "house" analogy.
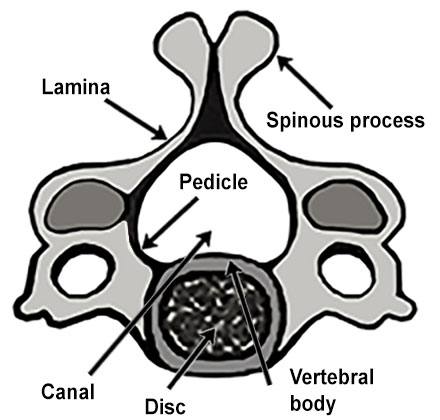
Illustration of cervical spine vertebra and disc.
If we break down the word “laminoplasty” into two parts: “lamino-“ and “-plasty” it is easier to understand the difference between other, similar words. The “lamino-“ portion shows which part of the body the procedure is performed on, in this case the lamina or “roof.” The root “-plasty” (from the Greek, plastia meaning “formed” or “molded), is similar to another word we hear commonly in everyday life: “plastic.” Plastic is a moldable material that can be made into all types of shapes and colors. Likewise, the “-plasty” portion of the word “laminoplasty” means that the lamina will be reshaped or molded into a new form.
Similarly, we can review the root words of laminectomy and laminotomy to illustrate their differences from a laminoplasty:
- “Laminectomy” ends with “-ectomy” instead of “-plasty.” In medical language (drawn from ancient Greek words), the root “-ectomy” means “to remove.” A “laminectomy” then means “to remove the lamina.” In some situations, it may be more beneficial to entirely remove the lamina portion of the bony spine than to reshape it.
- The word “laminotomy” contains a different root: “-otomy,” meaning “to make a hole.” A “laminotomy” then makes a small hole in the lamina, instead of removing the entire structure.
What are the surgical alternatives to cervical laminoplasty?
Cervical laminoplasty is only one of various procedures a spine surgeon can use to create space in a compressed spinal canal. One of the benefits of laminoplasty over other procedures is that it can preserve most of the natural motion of the cervical spine. In cases where a laminoplasty is not appropriate for a particular patient, or if they are interested in a different method of treatment, several other surgical options for spinal decompression are available, such as a laminectomy or discectomy. Alternative procedures include the following:
- Cervical laminectomy or laminoforaminotomy are other surgeries used to decompress the cervical spinal cord and its roots from the back (posterior) of the neck. A laminectomy is more extensive and is typically done together with a fusion procedure. A laminoforaminotomy is performed to relieve pressure on a specific nerve root, a common cause of cervical radiculopathy. Depending on your symptoms, you should discuss these options with your surgeon.
- Other options include approaching the patient’s cervical spine from the front (or anterior). Anterior cervical discectomy and fusion (ACDF surgery) can be performed in a minimally invasive way through the front of the neck to relieve pressure on the spinal cord and roots. This type of procedure may be necessary if the patient’s neck has deformity or other unfavorable alignment. Because this procedure involves fusing of the bones together, it does not preserve motion of the spine like a laminoplasty.
- Lastly, another option approaching from the front of the neck is a total disc replacement (TDR). As with a laminoplasty, one of the goals of this procedure is to preserve the natural motion of the spine. Rather than fuse the bones together, the diseased disc material between the bones is removed and replaced with a special, mobile implant. This procedure can relieve pressure on the spinal cord and its roots in addition to preserving motion. TDR is highly specialized and should be used in appropriate situations. This should be discussed with your surgeon.
Is cervical laminoplasty major surgery?
To be safely performed, cervical laminoplasty does require general anesthesia (in which the patient is completely asleep), and patients typically spend one or two nights in the hospital before recovering at home. At HSS, we consider the decision to have any surgery to be an important event a person's life. For many people, this is their first time having surgery of any kind, and so we always work to our make patients feel confident, comfortable, and assured of their safety prior to having their procedure.
Is a cervical laminoplasty painful?
Cervical spine surgeries performed on the back of the neck tend to be more uncomfortable than procedures performed through the front of the neck. Over-the-counter medicines, anti-inflammatory medications, muscle relaxers, and judicious use of opioid medications are used to make patients comfortable during their recovery. Most patients are able to discontinue opioid medications after a few days, and some patients find they need no opioids at all to manage postsurgical pain.
How long does a cervical laminoplasty take?
Cervical laminoplasty can be performed on its own or with other procedures (such as laminectomies) and on either one or several vertebrae at a time, so timing can vary. In most cases, the surgical time is between two and three hours, however this does not include time for anesthesia, safely positioning the patient, and awakening from anesthesia.
What is the recovery time for a cervical laminoplasty?
Patients typically spend one or two nights in the hospital before continuing to recover at home. Most surgeons will have their patients wear a soft, foam collar for one to two weeks for support. Muscle soreness in the neck may persist for several weeks, however this improves with time. Vigorous activity such as high-impact exercise will be limited for the first several weeks but can be resumed after four to six weeks. This should be discussed with your surgeon, who may have a specific, individualized protocol for you to follow.
Do you need physical therapy after a laminoplasty?
Physical therapy after cervical laminoplasty is not required but is often useful and prescribed by the surgeon. After the soft tissues have appropriately healed, a physical therapy regimen can be started to strengthen the neck and increase range of motion. Patients should consult with their surgeon about their postoperative protocols.
Is there any activity restriction after laminoplasty?
Some level of restriction is necessary immediately after surgery to allow the soft tissues to heal. Vigorous activities, such as running or weightlifting, should be avoided for the first several weeks. Low-impact exercise such as using an elliptical or stationary bicycle can be performed with no issues. Driving should be avoided if the patient is taking opioid pain medication, but otherwise can be resumed after one to two weeks as advised by your surgeon. Most patients return to unrestricted activity by four to six weeks after their surgery, however you should discuss this with your surgeon. There are no long-term restrictions after the surgical site has healed.
How successful is cervical laminoplasty?
Cervical laminoplasty can be performed for several different conditions. In recent studies cervical laminoplasty has been shown to have similar success to ACDF surgeries for treatment of cervical stenosis.
What risks or complications can occur with cervical laminoplasty?
All surgical procedures carry some general risks, including infection, bleeding and damage to surrounding structures. Compared to cervical spine surgery performed through the front of the neck (such as ACDF), the risk of infection is higher in surgeries performed through the back of the neck. This risk is still very small and can be managed with antibiotics and wound care if it occurs. In severe cases, an infection may require a second operation to help cure the infection.
Some blood loss is expected during the surgery. The amount is small, however, and this requires no treatment. Hematomas (collections of blood underneath the skin) can occur but don't usually require additional surgery. After most laminoplasty procedures a surgeon will leave a surgical drain in place to prevent a hematoma.
Because this surgery involves passing delicate surgical tools near the spinal cord, there is risk of damage to the cord itself or to the tissue that houses it, called the dura. In very rare cases, the dura can be torn, leading to a leakage of cerebrospinal fluid. This is treated with direct repair of the tear in the dura but may require a prolonged hospitalization to treat. Direct damage to the cord is exceedingly rare and may result in paralysis.
Lastly, an event that is unique to surgery involving the cervical spine is known as a “root palsy.” This commonly effects the fifth cervical root (C5), which gives motor power to the shoulder and biceps muscles. When the spinal cord is relieved of pressure the C5 root may stretch, resulting in a temporary dysfunction of that root. This can occur immediately after surgery or in a delayed fashion. In the vast majority of cases, this palsy recovers on its own but should be closely monitored by your surgeon.
Does cervical laminoplasty weaken the spine?
There is no weakening of the cervical spine after this procedure. Cervical laminoplasty does not involve removing any bone but making delicate cuts in the bone to reshape it. Once the soft tissues have healed around the reshaped bone the cervical spine functions normally.
Updated: 10/30/2022
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Associate Professor of Clinical Orthopedic Surgery, Weill Cornell Medical College
Attending Orthopedic Surgeon, Hospital for Special Surgery
Assistant Professor of Orthopedic Surgery, Weill Cornell Medical College




