Lumbar Laminectomy: Spinal Decompression Surgery of the Lower Back
Lumbar laminectomy is a type of spinal procedure which aims to relieve stenosis (narrowing of the spinal canal) or other forms of compression of the spinal canal at the level of the low back (lumbar spine).
What is a lumbar laminectomy?
Lumbar laminectomy is a common spinal procedure which involves partial or complete removal of the lamina from the lumbar spine in order to relieve compression of the neural elements within the spinal canal due to lumbar stenosis or other forms of spinal compression.
Spine anatomy
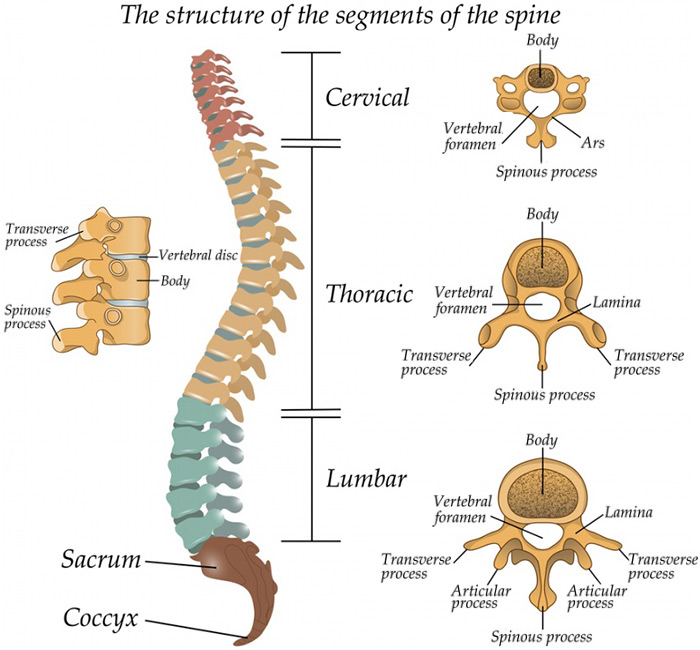
The spinal cord extends from the base of the brain and enters the spinal canal – a protective space within our bony spine.
The spine is divided into three sections, named for their location and function:
- The cervical spine composes the body’s neck and allows body to turn the head in many directions.
- The thoracic spine supports the rib cage, protecting the heart, lungs, and large vessels.
- The lumbar spine connects the torso to the pelvis and allows the body to bend, flex, and twist around the torso.
The mechanics of lumbar stenosis
Looking at the spinal canal in cross section, the lamina forms the “roof” of a house where the spinal canal sits inside the house. The “floor” is formed by the vertebral body and the “walls” are the pedicles, which connect the vertebral body to the lamina.
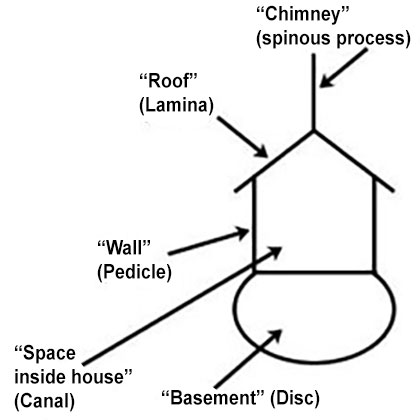
Diagram of "house" analogy.
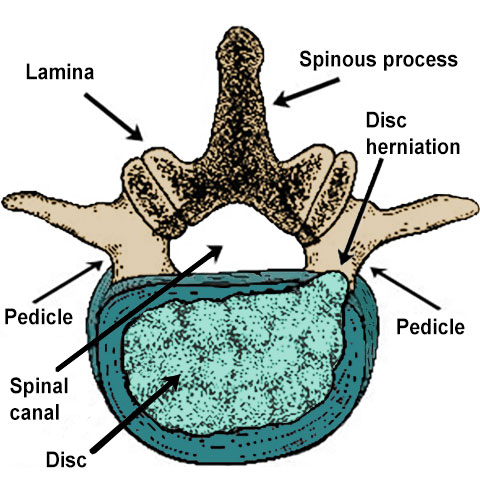
Illustration of lumbar spine vertebra showing a disc herniation.
Lumbar stenosis, or narrowing of the spinal canal in the lower back, is commonly due to degenerative processes (normal wear and tear from years of use) in the spine, also called spondylosis. This leads to the thickening of soft tissues and development of bony spurs which encroach on the space available for the spinal canal. Patients with lumbar stenosis may have symptoms that include back pain, leg pain, weakness, and changes in sensation. A laminectomy removes the bony roof as well as the thickened, swollen soft tissues forming the “roof” of the house allowing the canal to expand and nerve roots to return to normal health.
Who is a good candidate for lumbar laminectomy?
Patients who have symptoms of lumbar spinal stenosis that are not relieved with conservative management or who display progressive neurologic decline are good candidates for lumbar laminectomy. Patients should be evaluated for signs or symptoms of spinal instability which may require additional procedures, such as spinal fusion, in addition to the laminectomy. This should be discussed with your surgeon who will review your medical history and examine images of your spine. (Find an HSS Spine surgeon who performs lumbar laminectomies.)
What is a lumbar laminectomy versus a laminotomy?
A laminectomy involves removal of both lamina of a spinal vertebra to provide a wider decompression of the spinal canal. A laminotomy, on the other hand, is a more targeted procedure which removes bone from only a small portion of the lamina. This is a minimally invasive procedure which aims to decompress only very specific points in the spinal canal. Each of these procedures may be performed alone for this purpose, or also as a method for accessing an injured spinal disc, such as in a microdiscectomy surgery.
Is a lumbar laminectomy painful?
All surgical procedures come with some degree of pain to the soft tissues, but these are often managed via several modalities around the time of surgery. Conversely, most patients find that any leg pain they were experiencing prior to surgery is relieved immediately after surgery.
Is lumbar laminectomy major surgery?
Compared to other spinal procedures, lumbar laminectomy involves less dissection, less time under anesthesia, and can be performed as an outpatient procedure in some scenarios. However, lumbar laminectomy surgery does involve passing surgical instruments around the delicate structures of the spinal canal. In addition, to safely perform the procedure, it often requires general anesthesia (in which the patient is completely unconscious). Some surgeons are investigating other forms of lighter sedation for similar procedures – you should have this discussion with your surgeon if you are interested.
How does a surgeon perform a lumbar laminectomy?
Lumbar laminectomy may be performed openly (with an incision in the back) or minimally invasively (using a tubular retractor or endoscope). The choice of which procedure is most appropriate varies according to each individual patient’s spine condition and other health factors. Minimally invasive techniques are typically reserved for those with less extensive disease.
What is an open lumbar laminectomy?
A conventional, open lumbar laminectomy involves a posterior (from the back) approach to the spine. An incision is made in the center of the back in line with the spine. Soft tissue including the spinal erector muscles (the large muscles lying on either side of the bony spine) are delicately dissected from the spine, revealing the lamina. Using specialized instruments, the bony lamina is carefully resected (cut and removed), taking care to protect the surrounding neural elements. Once the bone and soft tissue have been removed, the surgeon will confirm that the area has been sufficiently decompressed.
What is a minimally invasive lumbar laminectomy?
A minimally invasive lumbar laminectomy uses a specialized tool call a tubular retractor or similar device to allow the surgeon to access the bony spine without having to dissect a large area of soft tissue. The retractor is placed over the appropriate area using X-ray or computer navigation and a small amount of tissue is removed to reveal the bony lamina. Using specialized tools, the bone is removed through the narrow tube. In some instances, the entire lamina can be removed through a single incision about 2cm to 3cm long (about 0.75” to 1”). Endoscopic techniques (using cameras and smaller incisions) may be utilized when appropriate.
Lumbar laminectomy animations
Posterior lumbar laminectomy
Posterior Lumbar Laminectomy with Instrumentation and Fusion
After removing bone during a posterior lumbar laminectomy, bone grafts can be added to fuse the vertebrae and support the spine. In case where there is spine instability, stabilizing instrumentation is added.
Posterior Lumbar Laminectomy with Fusion, without Instrumentation
In patients who have little or no instability, where the vertebrae, discs, and surrounding tissues fit tightly together, instrumentation is not necessary and the bone grafts can sufficiently stabilize the spine.
How long does a lumbar laminectomy take?
Lumbar laminectomy can be performed at one or more spinal levels (vertebrae), depending on the extent of the disease that needs to be addressed. The actual surgical time for a single level (one vertebra) can range between 30 and 90 minutes. This does not include time taken to ensure safe practices in the operating room, including inducing anesthesia, positioning the patient on a specialized bed, and safely waking up from anesthesia after the procedure is completed.
In many situations, a lumbar laminectomy can be performed as an outpatient procedure, meaning that they are able to return home the same day as surgery to recover. Patients are generally able to get up and walk immediately after surgery, and most find that leg pain they were experiencing prior to surgery is relieved immediately.
What is the recovery time for a lumbar laminectomy?
In some cases, patients can return home on the same day to recover. In cases where patients require surgery in multiple levels of the spine, they may spend one or two nights in the hospital prior to recovering at home. Patients can perform normal activities of daily living such as bathing, dressing, eating, and short, gentle walks immediately after surgery. Depending on your surgeon’s plan you may start physical therapy activities three to six weeks after surgery.
Do you need physical therapy after a laminectomy?
Physical therapy after a lumbar laminectomy may be beneficial for patients who have dealt with pain and poor function prior to surgery. Physical therapy will help to restore confidence, strength, and balance for patients after surgery. Depending on your recovery and your surgeon’s plan will determine when is optimal to begin therapy after surgery.
How soon can you walk after a laminectomy?
Most patients are able to walk immediately after surgery, depending on how well they were able to function prior to surgery.
How successful is lumbar laminectomy?
Lumbar laminectomy performed in the right patient at the right time is generally highly successful and can provide immediate, long-lasting relief from symptoms of spinal stenosis. In rare cases where a patient has residual pain after surgery, they may benefit from consulting with a pain management specialist.
How many years does a laminectomy last?
Laminectomy for lumbar spinal stenosis has been extensively studied. There is good, long-term evidence that the benefits of lumbar laminectomy are durable. However, there is risk of continued degeneration at spinal levels (vertebrae) above or below the area where surgery was performed. This can progress to stenosis in vertebrae which did not undergo surgical treatment.
What risks or complications can occur with lumbar laminectomy?
All surgeries carry some risk, including broad categories such as infection, bleeding, and damage to nearby structures. The infection risk of lumbar laminectomy is very small: less than 1%. Careful attention is paid to sterility during the procedure and patients are given antibiotics as a precaution during surgery. Bleeding is encountered as part of normal surgery and is meticulously controlled by the surgeon. In some cases, a surgeon may place a surgical drain – a device which prevents a buildup of fluid including blood and other fluids in the area of the surgery.
In very rare cases a hematoma (a collection of blood beneath the skin) can form in the area of surgery which may require another surgery to remove. Lastly, because this surgery involves passing surgical devices near the spinal canal, there is a small risk of injury to the thecal sac (the sack which contains the nerves and spinal fluid) or individual nerve roots themselves. A tear or puncture of the dura requires repair and may require a prolonged hospital stay. While not common, this remains a reported risk. Occasionally, nerve roots can become irritated as a result of surgery, but this can be treated with anti-inflammatory medications.
Does lumbar laminectomy weaken the spine?
Lumbar laminectomy requires careful removal of bone from the spine to decompress the spinal canal. Care is taken to preserve a bridge of bone between the spinal levels, which provides stability to the spine. In rare cases this bridge of bone may fracture during surgery or afterwards, which should be monitored for appropriate healing. The removal of bone from the back of the spine does not mean that there is no protection for the spinal canal. The large back muscles (erector spinae) and other connective tissue covers the area where the bone was removed, and scar tissue is also formed. Together these provide adequate protection for the spinal canal.
What are the surgical alternatives to lumbar laminectomy?
Alternatives to a lumbar laminectomy should be determined by discussion with your surgeon. There are a variety of methods of spinal decompression surgery to treat stenosis, including targeted laminotomy, conventional laminectomy, and minimally invasive laminectomy techniques. If a person’s stenosis is caused in part by a herniated disc, a laminectomy may be performed in conjunction with some type of discectomy. Exactly which technique(s) are best for your particular condition should be selected between you and your surgeon.
Updated: 10/31/2022
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Assistant Professor of Orthopedic Surgery, Weill Cornell Medical College
Attending Orthopedic Surgeon, Hospital for Special Surgery
Assistant Professor of Orthopedic Surgery, Weill Cornell Medical College