Herniated Disc (Bulging Disc): Symptoms and Treatment
Intervertebral discs are rubbery cushions between the segmental bones of the spine (vertebrae). They act as shock absorbers and provide the normal flexibility of the spinal column. Each disc’s normal location is directly adjacent to the spinal nerves.

- What is a herniated disc?
- Why does a disc herniate?
- Which discs herniate most frequently?
- What are the symptoms?
- What does it feel like?
- Will it heal on its own? How long does it take?
- When should I see a doctor?
- What type of doctor?
- Can you see a herniated disc on X-ray?
- How is a herniation diagnosed?
- What is the best treatment?
- What is the surgery?
What is a herniated disc?
A herniated disc (also known as a disc herniation and sometimes called a "slipped disc") occurs when a piece of a spinal disc bulges or ruptures and slips out of place, squeezing a spinal nerve. This may cause leg pain, leg weakness, leg numbness, cauda equina syndrome, and/or low back pain.
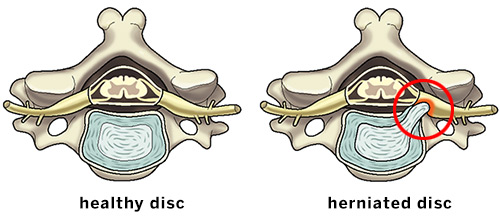
Illustrations of the axial (overhead) view of a healthy cervical disc and a herniation putting pressure on a spinal nerve.
Why does a disc herniate?
Unlike most other parts of the body, lumbar discs begin to deteriorate (degenerate) at a young age. Many patients in their twenties will have disc degeneration revealed on X-rays or MRI, and virtually 100% of elderly people have multiple degenerated discs.
As discs degenerate, they lose their water content and elasticity, and the retaining wall around the disc (annulus) begins to fissure or tear. Pieces of the deteriorating disc can then protrude out (herniate) through the leaking annulus. As the disc degenerates, low back pain may result. If herniated disc fragments compress a spinal nerve, it may result in leg pain, weakness, and/or numbness.
Discs often herniate without any unusual traumatic event, but in some cases, there may be contributing factors such as excessive weight, poor posture, heavy lifting, or trauma.
Which spinal discs herniate most frequently?
Although a herniation can occur in any section of the spine, herniated discs in the lumbar (low back) and cervical (neck) spine are the most common. Symptoms may include low back or neck pain, along with pain radiating into the leg ("sciatica") or arm, along with weakness and/or numbness. A herniated disc in the neck can cause a condition known as cervical radiculopathy.
Animations: Cervical and lumbar disc herniations
What are the symptoms of a herniated disc?
Because a herniated disc often compresses nerves at the point where they exit the spine, the symptoms people usually notice first are sensations caused by neuropathy (nerve dysfunction or damage). Pain and/or feelings of numbness or tingling may be felt in the neck or lower back but also frequently radiate outward to the extremities. For example, cervical disc herniations (in the neck) can cause cervical radiculopathy, with pain or tingling radiating from the neck or shoulder down the arm. In lumbar herniations, the sensations may radiate from the low back and down the leg by way of the sciatic nerve (commonly called “sciatica”).
More significant symptoms related to nerve damage include muscle weakness or, more rarely, bowel or bladder function.
What does herniated disc feel like?
A bulging disc may cause no sensation at all if it is not pressing on an adjacent nerve. When it does, a wide variety of pains or neuropathies may be felt, depending on which disc or discs are affected and the severity of the associated nerve compression. People often describe sharp or burning pain in the spine and/or the extremities. Many people also describe the feeling as an electric type “shocking” pain that is commonly associated with sciatica. Some may feel also numbness or tingling rather than pain, while others may feel both intermittently.
The location of these sensations may vary. Some people feel them only in the neck or back, or outward to the extremities. Others may feel sensation only in an arm or leg, with the neck or back unaffected. If a person with a herniated disc also has pain or numbness due to an unrelated condition of the extremity – such as rotator cuff tendinopathy in the shoulder or a compressed peripheral nerve in the outer arm, such as carpal tunnel syndrome – it can sometimes be complicated to determine which conditions are causing which particular sensations and further testing may needed to better evaluate which condition is causing the symptoms such as other physical examination maneuvers or a nerve test.
Will a herniated disc heal on its own? How long does it take?
Most cervical and lumbar disc herniations go away on their own without any treatment as the disc has the ability to resorb. The exception to this is in cases of cauda equina syndrome in which there is severe back and leg pain usually accompanied with loss of bladder or bladder function and immediate treatment should be sought at a local emergency room.
How do I know if my herniated disc is serious? When should I see a doctor?
You should see a doctor as soon as possible if you suspect a herniated disc and experience significant numbness accompanied by muscle weakness or dysfunction in your bladder or bowels. These symptoms can indicate possible nerve damage that may become permanent if not addressed. Even absent of such symptoms, if you experience significant pain or frequent numbness, you should seek an evaluation to rule out other injuries or conditions and determine the correct path for treatment.
What type of doctor treats herniated disc?
Several types of doctors can treat herniated discs. You may first see your primary care physician to describe the symptoms that you are experiencing. Treatment typically starts with anti-inflammatory medications and physical therapy. Strong pain medication such as opioids should be avoided. If the condition does not improve, you may be referred to a physiatrist or pain management physician for further treatment. Lastly, if there is no improvement in symptoms after such treatment, you may see an orthopedic spine surgeon to discuss whether surgical intervention may be needed.
Can you see a herniated disc on an X-ray?
An X-ray is best used to evaluate the skeletal structure and alignment of the spine. A herniated disc cannot be visualized on a plain X-ray. A plain X-ray will still typically be performed during the evaluation to help rule out other potential causes of pain, but if a bulged disc is suspected, other types of imaging will be ordered.
How is a herniated disc diagnosed?
Only a medical professional can diagnose a disc herniation. A thorough medical history and physical examination can point to the possibility of a disc herniation. The diagnosis can be confirmed by special tests such as MRI and/or CT myelography (myelogram). To differentiate between other possible causes of neuropathy, an EMG may also be ordered.
What is the best treatment for a herniated disc?
For persistent, painful herniations, treatment begins with the least invasive options, such as anti-inflammatory medications and physical therapy. If symptoms continue, interventional injection therapy is often the next step. This can include one or more of the following: epidural steroid injections, nerve root block, facet joint injection, SI joint injection.
The use of orthobiologic regenerative medicine treatments, such as platelet-rich plasma (PRP) or stem cell injections, is an active area of research. There is currently no consensus to recommend their use in treatment of a herniated disc, however, and they may increase the risk of infection or even worsen the herniation. But their prospective use is an active area of investigation of continued research.
Spine surgery is generally a last resort when conservative treatments fail. However, there are exceptions. For example, in a patient with a lumbar disc herniation who is experiencing significant weakness in leg muscles, early surgery may be recommended to minimize the possibility of permanent nerve damage and persistent leg weakness. Any worsening muscle weakness should be discussed with your surgeon.
What is the surgery for a herniated disc?
There are numerous procedures, depending on the particular herniation or herniations. Lumbar microdiscectomy surgery (microdecompression) typically provides excellent relief for complications caused by herniated discs in the lower back. For those who do not get relief or have recurrent symptoms, a revision decompression may be offered, or a disc replacement or spinal fusion may be recommended depending on other symptoms being experienced. In the cervical spine, disc herniations that require surgery can be treated with a posterior laminoforaminotomy, disc replacement, and cervical spinal fusion.
Explore the content below to learn more or find a find a doctor at HSS who treats disc herniations.
Herniated disc articles
Read more about back pain and slipped disc conditions.
Herniated disc treatment articles
Learn about different forms of surgical and nonsurgical treatment of herniated discs.
- Epidural Steroid Injections: Frequently Asked Questions
- Spinal Cord Stimulator – A Compelling Treatment Technique for Chronic Pain
- ACDF Surgery: Anterior Cervical Discectomy and Fusion
- Spine Surgery: Minimally Invasive Lumbar Discectomy / Percutaneous Disc Removal (PDR)
- Spine Surgery: Posterior Cervical Laminotomy
- Lumbar Fusion
- ALIF Surgery: Anterior Lumbar Interbody Fusion
- TLIF Surgery: Transforaminal Lumbar Interbody Fusion
- PLIF Surgery: Posterior Lumbar Interbody Fusion
- Microdiscectomy: Surgical Treatment for a Herniated Disc
- Minimally Invasive Lower Back Surgery for Disc Degeneration: The Anterolateral (Side) Approach
Articles on related topics
Herniated Disc (Bulging Disc): Symptoms and Treatment Success Stories
In the news
Updated: 12/4/2024
Reviewed and edited by Kyle W. Morse, MD
References
- Bailey CS, Rasoulinejad P, Taylor D, Sequeira K, Miller T, Watson J, Rosedale R, Bailey SI, Gurr KR, Siddiqi F, Glennie A, Urquhart JC. Surgery versus Conservative Care for Persistent Sciatica Lasting 4 to 12 Months. N Engl J Med. 2020 Mar 19;382(12):1093-1102. doi: 10.1056/NEJMoa1912658. PMID: 32187469. https://pubmed.ncbi.nlm.nih.gov/32187469/
- Elabd C, Centeno CJ, Schultz JR, Lutz G, Ichim T, Silva FJ. Intra-discal injection of autologous, hypoxic cultured bone marrow-derived mesenchymal stem cells in five patients with chronic lower back pain: a long-term safety and feasibility study. J Transl Med. 2016 Sep 1;14(1):253. doi: 10.1186/s12967-016-1015-5. PMID: 27585696; PMCID: PMC5009698. https://pubmed.ncbi.nlm.nih.gov/27585696/
- Jerome MA, Lutz C, Lutz GE. Risks of Intradiscal Orthobiologic Injections: A Review of the Literature and Case Series Presentation. Int J Spine Surg. 2021 Apr;15(s1):26-39. doi: 10.14444/8053. Epub 2021 Apr 21. PMID: 34376494; PMCID: PMC8092939. https://pubmed.ncbi.nlm.nih.gov/34376494/
- Al Qaraghli MI, De Jesus O. Lumbar Disc Herniation. [Updated 2023 Aug 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560878/
- Weinstein JN, Lurie JD, Tosteson TD, Tosteson AN, Blood EA, Abdu WA, Herkowitz H, Hilibrand A, Albert T, Fischgrund J. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2008 Dec 1;33(25):2789-800. doi: 10.1097/BRS.0b013e31818ed8f4. PMID: 19018250; PMCID: PMC2756172. https://pubmed.ncbi.nlm.nih.gov/19018250/
- Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, Herkowitz H, Fischgrund J, Cammisa FP, Albert T, Deyo RA. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006 Nov 22;296(20):2451-9. doi: 10.1001/jama.296.20.2451. PMID: 17119141; PMCID: PMC2562254. https://pubmed.ncbi.nlm.nih.gov/17119141/

