Rheumatoid Arthritis of the Foot and Ankle: An Overview
Adapted from a presentation to the Inflammatory Arthritis Support and Education Programs
Rheumatoid arthritis (RA) is a chronic autoimmune disease that attacks multiple joints in the body.

- Which joints are affected by rheumatoid arthritis?
- Can rheumatoid arthritis affect your foot and ankle?
- What are the symptoms of RA in the foot and ankle?
- How can I tell if my foot pain is caused by rheumatoid arthritis?
- What kind of doctor can treat RA of the foot and ankle?
- How is rheumatoid arthritis in the foot or ankle treated?
- How can rheumatoid arthritis in the foot be treated without surgery?
- What surgery is there for rheumatoid arthritis of the foot and ankle?
Which joints are affected by rheumatoid arthritis?
RA commonly affects small joints in the hands, wrists and feet, but it can also affect the ankles and larger joints such as knees or elbows.
Can rheumatoid arthritis affect your foot and ankle?
Rheumatoid arthritis in the foot and ankle is common. RA often starts in the small joints of the hands, wrists and feet. More than 90% of people with RA acquire foot and ankle symptoms over the course of the disease. In about 20% of patients, foot and ankle symptoms are the first signs of RA.
The joints of your body are covered with a lining known as synovium that lubricates the joint and makes it easier to move. In RA, the immune system attacks your body’s own tissues, including the synovium. It swells, gets inflamed, and destroys the surfaces of the bones that comprise the joint, along with the ligaments and other tissues that support it. Damaged, weakened ligaments can lead to claw toes or hammertoes. Bones can also lose density and become soft. Bone density conditions (osteopenia and osteoporosis) can cause stress fractures or bone collapse.
What are the symptoms of rheumatoid arthritis in the foot and ankle?
The most common symptoms are pain, swelling and stiffness. While osteoarthritis of the foot or ankle most often affects one joint, RA usually occurs in both feet, typically in the same joint on each foot. Here’s a table that gives you an idea of how RA presents in your feet.
| Part of the foot | Where it is/What it does | Early signs/symptoms | Later-stage symptoms |
|---|---|---|---|
| Ankle | Provides up/down motion of the foot. | Trouble with ramps and inclines. | Painful to walk or stand. |
| Hindfoot | Heel region of the foot − main function is to perform side-to-side motion of the foot. | Hard to walk on uneven ground, grass or gravel. | Alignment of foot may shift as bones move out of their normal positions; can result in pain in posterior tibial tendon (main tendon that supports the arch) and/or acquired flatfoot deformity. |
| Midfoot | Top of the foot. | Ligaments that support the midfoot become weak, and this can lead to collapsed arches. . | Once the arch collapses, the front of the foot may start to point outward. RA also damages the cartilage, causing arthritic pain. Over time, the shape of foot can change. For example, large bony bump on the arch can appear. |
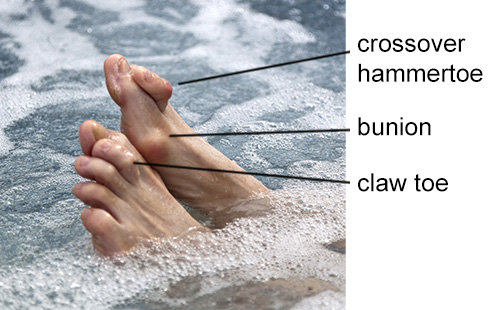
| Forefoot | Toes and ball of feet. | Changes include bunions, claw toes, and pain under ball of foot. While each of these is common, in RA the problem is compounded as they are combined. | The bunion is usually severe, and the big toe crosses over the second toe. There can be painful bumps on the ball of the foot causing calluses. These bumps occur when bones in the midfoot are pushed down from joint dislocations in the toes. Dislocations of toes 2-5 cause them to become prominent on the top of the foot, creating claw toes that become fixed and rigid. In severe cases, ulcers can form from the abnormal pressure. |
Can rheumatoid arthritis cause problems with tendons?
Yes. Tendons surround the joints of the foot and ankle. Often, a tight Achilles tendon worsens a flatfoot condition, so, exercise as best you can to help keep tendons flexible and strong.
How can I tell if my foot pain is caused by rheumatoid arthritis?
First, your healthcare team will talk to you about your symptoms, discuss your health, and review your medical history. Then your doctor will perform an exam of your foot and ankle, and then possibly order tests.
The exam
Your doctor will check your skin for calluses. The most common place for these is on the ball of the foot. They will look at your foot’s shape. Are there bunions, hammertoes, claw toes or flatfeet? Are the joints still flexible or are they stiff?
In more advanced RA, there may be a total loss of cartilage and the joints could get very stiff. Do your joints feel tender with pressure? Your doctor will apply gentle pressure at your joints to figure out which ones are involved and need treatment.
Tests
Based on what your doctor finds, they may order some tests to get a clear image of what’s going on in order to decide how best to treat your foot.
These tests may include X-rays to show the position of the bones. They may ask you to bear weight on the foot during the X-ray to see what the bones look like during normal use. They may also order computerized tomography, also known as a CT scan, of your foot. These special, cross-sectional images can provide a closer look at each joint when the foot is severely deformed.
MRI (magnetic resonance imaging) scans show soft tissue, ligaments and tendons, and can identify if they are inflamed (tendonitis) or torn.
What kind of doctor can treat rheumatoid arthritis of the foot and ankle?
If your primary care doctor suspects you have rheumatoid arthritis, they may refer you to a rheumatologist. It could also be that you have another, less inflammatory type of arthritis, but a rheumatologist is best able to make a diagnosis. If a rheumatologist determines you have osteoarthritis instead, they may recommend you meet with an orthopedist (orthopedic surgeon) who specializes in foot and ankle conditions. Rheumatoid arthritis patients who experience inflammation in the foot and ankle are often treated by a multidisciplinary team that includes their primary care physician, a rheumatologist, a podiatrist and an orthopedist.
Other healthcare clinicians who may be of help
How is rheumatoid arthritis in the foot or ankle treated?
There is no cure for RA, but there are many nonsurgical and surgical treatment options that enable people to manage pain, stay active, and live full lives. Medical/conservative management is the mainstay. Surgery is a last resort if medical treatments are unsuccessful.
How can rheumatoid arthritis in the foot be treated without surgery?
Orthopedic treatment may provide symptom relief but does not stop the disease process. Still, many patients will have symptom relief without surgery. One such option is a steroid injection. Corticosteroids can reduce inflammation and pain in the short term. Your doctor may also prescribe disease modifying anti-rheumatic drugs (DMARDs), such as methotrexate. There are also NSAIDs (nonsteroidal anti-inflammatory drugs) such as ibuprofen or naproxen which can reduce pain and inflammation. Always check with your doctor before you take any medication- even over the counter.
Sometimes, it’s the simple things such as rest or icing the joint that may be the most effective. Rest your foot by taking a break from things that make the pain worse. Place ice on the area of pain for 20 minutes. Always wrap the ice pack in a wash cloth or something so that it does not contact your skin directly.
Relief may also come from things you wear. Firm shoes with a wide toe box and arch support are usually best. An orthotic is a shoe insert that can help to reduce pressure and decrease pain and calluses from forming. Watch out for hard orthotics as they may actually cause more pain. A customized, prescription orthotic is made of softer material and best relieves pressure on the foot. If you need support at the back of foot and ankle, a lace-up ankle brace made of plastic or leather can help.
Depending on the damage to cartilage, your doctor may suggest surgery.
What surgery is there for rheumatoid arthritis of the foot and ankle?
Fusion surgery in the foot or ankle is the most common. These procedures provide rheumatoid arthritis foot and/or ankle pain relief, but can compromise flexibility. Other procedures include total ankle replacement and toe joint resections. The appropriate option depends on each patient’s condition and the joints that are affected.
Ankle surgery for RA
The most common surgery for RA is fusion. This is when two bones that form a joint are fused together using hardware such as screws and plates. An ankle fusion relieves pain but results in loss of the up-and-down motion of the ankle. This requires nearby joints to compensate for this loss of motion.
Total ankle replacement is another surgical option. Patients with other joint issues around the heel or those who already had fusions may be well suited for ankle replacements. It avoids adjacent joint arthritis caused by overcompensation for loss of movement in another joint.
Midfoot surgery for RA
Midfoot fusion is the most reliable surgery for the joints of the midfoot. It helps to restore the arch, lessen prominences, reduce pain, and improve chance for normal footwear.
Forefoot surgery for RA
For forefoot issues, the options range from joint sparing procedures that preserve motion to fusion of the toes. The appropriate surgery depends on your flexibility and the health of your cartilage. These procedures can provide good function and improve odds for normal footwear.
Preparing for foot and ankle surgery and your recovery
Many medications that help with RA affect the body’s ability to heal and fight infection. Your surgeon can work with your rheumatologist to decide what to stop taking prior to surgery and when to resume the medication(s). Typically, foot surgeries require that no weight be placed on the foot for about two-six weeks. Since these surgeries are planned, it is good to know this in advance to prepare your home and line up your support system to help you as you recover.
The takeaway
The best means to manage your RA are through medical care and newer medications. Surgery can help but should be a last resort.
The main goal is to get rid of the pain. Keep in mind, even if one finds relief and can begin to wear sandals or mid height heels with ease, it is still best that these types of shoes are not worn often.
This article is based on a presentation by Dr. Behrens to the HSS Early RA Support and Education Program.
Posted: 8/3/2021
Authors
Attending Orthopedic Surgeon, Hospital for Special Surgery
Assistant Professor in Orthopedic Surgery, Weill Cornell Medical College
Laura Jasphy, Ed.D
Senior Clinical Social Worker, Hospital for Special Surgery

