Hip Pain Causes, Conditions and Treatments
- Causes of hip pain
- Where is your hip pain?
- Common conditions that cause hip pain
- When to see a doctor for hip pain
- What kind of doctor should I see for my hip pain?
- How do I know if I need hip surgery?
- What kind of surgeon does hip surgery?
Causes of hip pain
Hip pain in adults may be caused by a wide variety of conditions that affect the bones or soft tissues that surround them. Mild, temporary discomfort in the hip can occur in individuals of all ages as the result of overuse of a muscle or tendon, for example, while training with weights or participating in sports or other recreational activities. In middle-aged and older adults, degenerative changes to and injury of cartilage and other soft tissues are likely to cause gradually increasing and longer lasting pain in the joint.
Anatomy of the hip
The hip is a ball-and-socket joint composed of two bones connected by cartilage, ligaments, tendons and muscles:
- the femoral head or tip of the femur (thighbone) is the ball
- the acetabulum, a cup on the side of the pelvis, is the socket
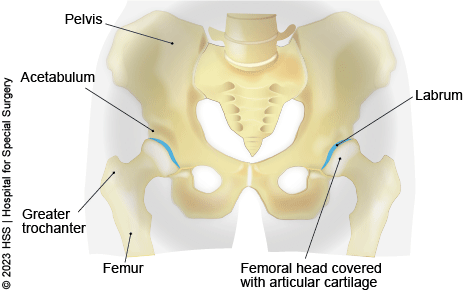
A protective layer of cartilage lines the ball and socket to allow the leg to glide smoothly backward, forward, and sideways. An additional ring of specialized cartilage in the acetabulum called the labrum further protects and stabilizes the joint.
Where is your hip pain?
The location of hip pain provides additional information about the underlying problem. For example, in older adults, pain that runs along the front of the hip as well as the thigh and groin suggests the presence of arthritis. Pain along the outer part of the hip may be due to bursitis – inflammation of the small fluid-filled sacs called bursae that provide cushioning around the hip joint.
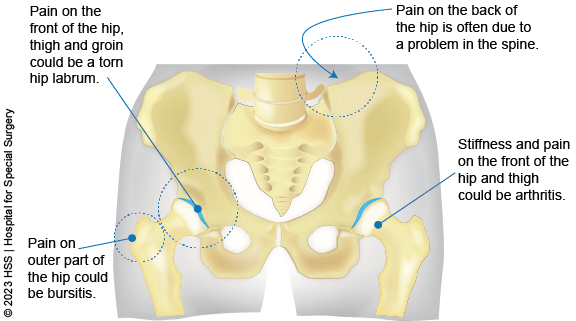
Pain that occurs in the back of the hip or buttock area is often due to a problem in the spine rather than the hip joint itself.
Common conditions that cause hip pain
Mild, temporary discomfort in the hip can occur in individuals of all ages as the result of overuse, for example, while training with weights or participating in sports or other recreational activities. A wide range of other non-traumatic conditions may be responsible for persistent hip joint pain. Some of the more common ones include:
Osteoarthritis of the hip
Among patients in their 50s, 60s, and older, osteoarthritis of the hip is among the most commonly seen. Osteoarthritis is diagnosed when either normal wear and tear, or an injury, damages the cartilage that lines the bones that make up the joint. Pain occurs when “bone on bone” contact is made without any cushioning. Patients with osteoarthritis often experience stiffness together with pain along the front of the hip and the thigh and groin. Osteoarthritis can come about from a variety of factors including genetics, wear and tear, injuries, and other lifestyle factors.
Less often, people of any age may develop some type of inflammatory arthritis, which can also affect the hip and cause pain or stiffness.
Hip labral tears
The labrum is a cartilaginous ring that covers the hip socket in the pelvis. A torn hip labrum (labral tear) causes front hip pain, as well as symptoms in the groin.
Stress fractures of the hip
A stress fracture – the result of pressure that is repeatedly placed on a bone – can be a source of significant hip pain. These fractures differ from those that occur with a traumatic injury and result in misalignment of the bone. Stress fractures can occur in individuals who do a lot of high intensity sports or running. However, people with poor bone quality are also at increased risk of this injury.
Soft tissue injuries of the hip
Conditions that affect the soft tissues include inflammation or injury to a muscle, ligament, tendon or bursa in or around the hip. The location of pain associated with injuries of soft tissues around the hip varies. For example, pain on the outer part of the hip may be due to a problem affecting the abductor muscles, which control sideways movement of the leg, or as a result of hip bursitis – inflammation in one of the bursae in the hip. (A bursa is small fluid-filled sac that provides cushioning in various joints.) A dislocated or subluxated hip can also damage soft tissues and cause pain.
Spinal conditions
Since the lower spine connects to the hip, various conditions of the lumbosacral spine may also present as hip pain. The most common example is sciatica resulting from a herniated disc or spinal stenosis, in which nerves that exit the spine become pinched, causing pain that may radiate to the hip as well as down the leg to the toes. A less common example is sacroiliitis – inflammation of the joint between the sacrum of the spine and the pelvis, which itself can have various causes.
The term hip-spine syndrome is used to describe a situation in which a person has conditions in the hip and the spine which are both causing pain, such as osteoarthritis of the hip and lumbar spondylosis. Diagnosing the precise cause of hip pain in such cases can be challenging, since the pain arises from two or more sources.
Hip infections
An infection in the hip joint, which can result from injury, spread from an infection in another part of the body, or result from a previous surgery, may produce pain in the front of the hip, though the location of symptoms may vary.
Avascular necrosis
Avascular necrosis (AVN, also known as osteonecrosis) is a less common source of hip pain that develops when blood flow to the femoral head (the upper end of the long bone in the thigh) is poor or absent, resulting in damage to the bone and eventual collapse of the head of the femur. In children, AVN may occur in a rare condition known as Legg Calve Perthes disease.
When to see a doctor for hip pain
People with mild hip pain often achieve relief with over-the-counter pain relievers, activity modification, rest, and icing the joint, and may not require further treatment. However, those experiencing pain that is increasing or which occurs when putting weight on the hip or while walking should seek prompt medical attention. Having an X-ray, physical examination, and, where needed, additional imaging, is the best way to ensure that the cause is not due to a fracture or other serious condition. Individuals who have undergone surgery for a hip replacement or other condition, and whose pain persists past the anticipated recovery period, should also seek medical attention.
Timely treatment of hip pain is an important way to prevent discomfort in other joints that can develop when patients compensate for an injury by altering the way they move or walk to alleviate pain.
Make an appointment if:
- You have persistent or intermittent hip pain.
- Performing a specific activity, such as running, causes recurring hip pain.
- You have experienced a loss in range of motion in your hip.
- Hip pain wakes you from sleep.
- Hip pain is accompanied by:
- swelling, tenderness in soft tissues around the joint, or redness in the skin in the region of the hip.
- popping or clicking sounds while walking or running
- weakness or instability, and stiffness or reduction in your range of motion
What kind of doctor should I see for my hip pain?
In most cases, you will want to first consult an orthopedist specialist. However, these physicians frequently specialize in specific types of conditions within orthopedics. If you suffered an obvious, acute injury to your hip, it is best to consult with a sports medicine surgeon or orthopedic trauma surgeon to learn whether you may need surgery.
For milder symptoms that began during exercise or physical labor, or which have no obvious cause, consider seeing a nonsurgical primary sports medicine physician or physiatrist to diagnose your condition.
If you are over age 50 and think you may be developing arthritis, you may opt to first see either a rheumatologist, an orthopedic surgeon specializing in hip replacement, or a metabolic bone specialist to learn whether you may be developing degenerative arthritis, osteoporosis or both.
At HSS, our Hip Preservation Service is a cross-disciplinary team of doctors and surgeons who work to help patients avoid or delay hip replacement surgery in favor of less invasive options whenever possible.
How do I know if I need hip surgery?
Many hip conditions do not require surgery and may improve after conservative treatments such as physical therapy, NSAIDs (nonsteroidal anti-inflammatory medications) such as ibuprofen, corticosteroids injections or other injection therapies.
What kind of surgeon does hip surgery?
An orthopedic surgeon (also known as an orthopedist) performs surgeries of the hip. However, since the hip is a complex system of bones, cartilage and other soft tissues, orthopedists frequently specialize in specific types of hip injuries or patient populations. At HSS, hip surgery is performed by subspecialists in multiple surgery services:
- The Orthopedic Trauma Service treats hip fractures and other acute injuries caused by high-impact events, such as work-related accidents, vehicle collisions or falls.
- The Adult Reconstruction and Joint Replacement (ARJR) service specializes in total and partial hip replacement and knee replacement. Hip replacements are primarily performed to treat hip arthritis, however they may also be appropriate procedures some fractures and other conditions.
- The Sports Medicine Institute performs surgeries to hip labral tears and other conditions.
- The Hip Preservation Service is a cross-disciplinary team of surgeons from all three of the above services, as well as nonsurgical doctors from Primary Sports and Physiatry. This team aims to help patients avoid or delay hip replacement surgery in favor of less invasive options whenever possible.
- The Pediatric Orthopedic Surgery Service surgeons treat hip conditions affecting growing children and adolescents, including hip dysplasia.
Hip disorders and injuries
Learn about various hip conditions treated at Hospital for Special Surgery.
- Avascular Necrosis (AVN, Osteonecrosis)
- Bursitis of the Hip
- Cartilage Injuries & Disorders
- Femoral Anteversion (Hip Anteversion)
- Femoral Retroversion (Hip Retroversion)
- Fractures of the Hip and Pelvis
- Hip Arthritis
- Hip Cysts
- Hip Dislocation
- Hip Dysplasia
- Hip Impingement
- Labral Tears of the Hip
- Outpatient Surgery: Frequently Asked Questions
- Sciatica
- Strained Hip
- Synovitis
- Tendinosis
- Tendon Injuries and Conditions
Hip pain treatments
Learn about various hip condition treatments available from Hospital for Special Surgery.
Updated: 11/1/2023
Reviewed and edited by Cynthia A. Kahlenberg, MD, MPH
